Welcome to the Virtual MS Center!
Ask any question you want about Multiple Sclerosis and one of our experts will answer it as soon as possible.
|
Here is My Question:
Are chemotherapy medications added to Tysabri for infusion? I noticed on my medical statements we are being charged for it. Answer: You should call your infusion center billing office to get more information on their billing procedures. Many centers bill infusions of all types, including steroid infusions, under a chemotherapy infusion code and this can be confusing when you receive the bill. This doesn’t mean that you are also receiving a chemotherapy. You doctor certainly would have been required to get your approval for any chemotherapy. Rip Kinkel, MD Question:
How is it determined when your RRMS changes its status to the progressive MS diagnosis ? I see my daughter's baseline decline, yet she still has the RRMS status. Answer: When a person develops progressive MS after an initial relapsing remitting course, we call this secondary progressive MS (SPMS). Determining the onset of SPMS is very difficult; in most cases we observe a patient at multiple visits over a period of time, usually 1-5 years, and eventually decide that they are now secondary progressive. There are certain features that suggest secondary progressive MS but all that is really required is progressive worsening of impairment without significant improvement or an alternative explanation over an interval usually in excess of 6 months. Typical but not required features of secondary progressive MS are the following:
Rip Kinkel, MD Question:
I've been diagnosed with PPMS, why do my symptoms wax and wane or disappear and others take their place? Answer: Primary progressive MS is differentiated from relapsing remitting MS by two clinical features: 1. The slow temporal course of symptom development 2. The lack of significant improvement Both relapsing remitting and primary progressive MS patients experience fleeting symptoms that come and go or symptoms that worsen with certain activities, illnesses or even the time of day; these signify neither a relapse nor progression. I have written previous blogs that explain the reason for these symptoms that come and go. Please refer to these blogs for an explanation. Let’s look at each of the characteristics that differentiate relapsing remitting and progressive MS more closely... Relapses are the acute or subacute development of new symptoms or worsening of old symptoms without improvement over hours to days usually with corresponding findings on examination by a neurologist; 80% of patients reach their worst deficits within 2 weeks and more than 90% within one month. At times the symptoms are so dramatic in onset that a relapse can be confused with a stroke. Symptoms and findings develop very slowly in primary progressive MS. They also tend to wax and wan considerably at the beginning but the overall pattern is one of continued worsening. The most typical symptom is a slowly developing abnormality in the way a person walks. One typical story we hear from patients and families at the time they are first seen by a neurologist sounds something like this: “I was always active until last year when I began to drag my right leg. Its been getting slowly worse and I finally agreed to see the doctor when I could no longer hide the problem and people at work were beginning to think I had a drinking problem. I thought it was just a bad hip but my primary doctor could find nothing wrong with my hip. I’ve actually been a little concerned for at least two years or at least since our family reunion 2 years ago last summer; we had a game of touch football and I started to stumble and trip after playing for about an hour. I just figured this was due to the hot weather and deconditioning. After this I began to notice decreasing endurance with my morning jogs and began to trip or drag my right leg after a few miles; eventually I stopped running altogether about a year and half ago" Contrast this description with a relapsing remitting MS description: “When I woke up last monday my right leg felt heavy and my right foot was tingling. At first I thought the right leg was still asleep but the symptoms persisted. Later in the day I noticed that the numbness and tingling had moved up the right leg to about thigh level and I kept tripping over my right leg when I walked too fast. It seemed a little better with rest that evening. The next day when I got out of bed I stumbled to the bathroom because of my right leg weakness and imbalance and could barely walk without assistance. Of course, this is when I decided to come to the emergency department. The symptoms continued to get worse and spread to the left leg over the next few days. Once they determined I had MS they treated me with IV steroids. I noticed some improvement by the following day and was ready to return to work 4 weeks later. I felt almost completely normal within 3 months” -Rip Kinkel, MD  I like the ease of disassembly of the Pride GoGo Traveller Elite http://www.pridemobility.com/gogo/gogoelitetraveller.asp and/or the Golden Technologies Buzzaround http://www.goldentech.com/products/buzzaround-lite/. When choosing a travel scooter also keep in mind the weight capacity of the unit and distance capability, as these vary - Tom Mellor, Assistive Technology Professional (ATP). To read more about Tom, Click Here This is an excellent question for which we do not have the data required for an adequate answer; let’s think this through together:
These are all answerable questions but they are difficult to answer since PML is so rare. Even in individuals with the highest risk (JCV antibody positive, prior immunosuppression and greater than 2 years of therapy), the incidence of PML is only between 1 and 2 %. Therefore, you have to study a lot of people on treatment (many 10s of thousands) before you accumulate enough cases of PML to know if the risk of PML over time changes with stopping and starting treatment. The best answer I can give you is the following: if Tysabri is the best therapy for you given your circumstances, then you should consider remaining on therapy or restarting therapy but only if you are willing to work with your MS specialist to mitigate against the risk of PML. There are many protocols in use that attempt to lower the risk of PML or detect it sooner so that it can be eradicated more easily. These protocols include: 1. Increasing the interval between infusions to every 6 or 8 weeks 2. Obtaining an MRI of the head every 4 months using a brief protocol without a contrast agent to detect early PML before the development of any symptoms 3. A combination of 1 and 2 above The use of drug holidays (i.e. stopping tysabri for at least 6 months before restarting) is done less often these days because of the risk of relapse within 3-6 months of stopping tysabri. None of these protocols are currently sanctioned by either the FDA or the company that makes Tysabri. This is true of many decisions that patients make with their doctors about treatment. For this reason it is most important for you to discuss these issues thoroughly with your current MS Specialist and find an approach to this problem that works well for both of you. -Rip Kinkel, MD PLEASE NOTE: The information/opinions on this site should be used as an information resource only. This information does not create any patient-HCP relationship, and should not be used as a substitute for professional diagnosis and treatment. Please consult your health care provider before making any healthcare decisions or for guidance about a specific medical condition. As we plan for the future of this website, we really want to know what you as readers want. Please take a few moments to complete this survey (click on the link below). Some of you may have already taken a similar survey (and thank you for your feedback, we are working on it!). We have added questions, so feel free to take the survey again so we are sure to have everyone's feedback.
https://www.surveymonkey.com/s/HealthCareJourneySurvey Tysabri can be switched to another MS medication but there are specific issues that must be addressed by you and your physician prior to any switches:
If you go to the search box for this site and type in Tysabri you will see more information that you might be interested in, such as the answer to a question about switching from Tysabri to Tecfidera. -Rip Kinkel, MD PLEASE NOTE: The information/opinions on this site should be used as an information resource only. This information does not create any patient-HCP relationship, and should not be used as a substitute for professional diagnosis and treatment. Please consult your health care provider before making any healthcare decisions or for guidance about a specific medical condition. Psychosis is usually defined as a thought disorder where the individual loses contact with reality, at least temporarily. Very brief episodes may be due to seizures. Associated symptoms of psychosis usually include delusions and hallucinations. Isolated psychosis is rare in MS but can occur and is amenable to the usual treatments used to treat psychosis associated with psychiatric disease. It is always most important to exclude a drug induced psychosis, particularly street drugs.
Psychotic behavior may be associated with bipolar disorder which in turn may occur more often in people with MS than in people without MS. Similarities between bipolar disorder and MS include age of onset, fluctuating nature of symptoms and white matter abnormalities, especially in the temporal lobes. As with all psychiatric symptoms in MS it is important to exclude drug effects. For instance manic behavior is fairly common with steroid treatments. Rip Kinkel The information/opinions on this site should be used as an information resource only. This information does not create any patient-HCP relationship, and should not be used as a substitute for professional diagnosis and treatment. Please consult your health care provider before making any healthcare decisions or for guidance about a specific medical condition.  Differentiating between Systemic Lupus Erythematosis (also called SLE or Lupus) and Multiple sclerosis can be very difficult. Both are essentially a clinical diagnosis, meaning there is no specific diagnostic test that differentiates between the two disorders. The good news is that verifiable lupus probably involves the central nervous system in less than 5% of patients, despite prior studies suggesting a larger percentage of lupus patients with central nervous system involvement. In my experience most patients with well documented Lupus who also have a characteristic history, exam and diagnostic evaluation for MS have both disorders. Similarities between Lupus and MS include the following:
Differences between Lupus and MS mostly reflect a different pathogenic mechanism of tissue injury; specifically, MS symptoms are caused by inflammatory demyelination within the brain tissue whereas lupus symptoms involving the central nervous system are pathologically related to immune mediated injury to small blood vessels (the vessel lumen becomes narrow and can close off) supplying oxygen and nutrients to an area of the brain. This difference is extremely important since the type of injury created by Lupus tends to be more severe with less recovery because the tissue is deprived of essential nutrients and oxygen (like a stroke), whereas significant recovery is more common in MS. Specific things to look for to help differentiate the two conditions include: Lupus eventually involves other parts of the body with symptoms like arthralgias, myalgias, a characteristic rash, livido reticularis, kidney, heart or pulmonary involvement Lupus as well as neuromyelitis optica should be considered with any case of severe optic neuritis associated with little recovery or complete longitudinally extensive transverse myelitis Lupus is less often associated with typical MS MRI findings likely periventricular and juxtacortical lesions but it can be difficult to separate the two by MRI If the evidence supports a diagnosis of lupus or both lupus and MS, this will effect how you are treated. It is important to avoid interferons since there are a number of studies implicating type I interferon pathways (the type triggered by treatment with beta interferons or alpha interferons) in the cause of Lupus and anecdotal evidence of worsening lupus in MS patients treated with interferons. In my opinion immunosuppressant and anti-CD20 therapy (rituximab) is the preferred option for these patients. The actual therapy recommended will depend on the situation but could include periodic steroids, azathioprine, mycophenolate, cyclophosphamide or rituximab. A newer therapy for MS called teriflunimide (Aubagio) could be strongly considered as well because of its mechanism of action. Many patients end up on combination therapies that may include Copaxone plus one of the agents previously mentioned. Treatment of this small group of patients is guided primarily by experience with little evidence to support one or another approach. I would recommend discussing the options thoroughly with your doctor and finding a neurologist experienced in the management of these conditions with or without the assistance of a rheumatologist. Rip Kinkel Question: What are the biggest challenges that patients and their families have with adjusting to MS? Since this is a virtual center, what technology would help families?
Answer: This is a very difficult question to answer with a single response. In fact the complexity of the both the question and the answer is the main reason for this website. The challenges adjusting to MS vary from patient to patient and over the course of the illness. The biggest challenge is learning to deal with uncertainly and incomplete information. The disease is so variable that it is difficult to predict either the course or the response to treatments. The best thing to do in this circumstance is to try and follow some simple rules: 1. Educate yourself and take an active approach in your care 2. Set defined goals beginning with those that are both most important and most attainable; in fact with every thing you do, whether it be taking a prescribed medication, going to the YMCA to work out or going back to school, try to develop short and long range goals. This allows you to become more actively involved and will enhance the chances for success. 3. Do not fixate on a particular solution until a problem has been fully analyzed and all information collected. Patients often come to me asking to get a particular medication or device or type of therapy and do not even tell me what problem they are trying to solve. This is most common with MS disease modifying therapies but can occur with almost request. When I ask them what problem they are trying to solve, examine them and explain the best options they are often amazed at the simplicity of the offered solutions. However, if they arrive determined to have their way, the outcome is usually less than satisfactory. 4. Break up time into useful blocks for reassessment of specific goals. For instance, if you just started a new medication for your MS consider the first 3 months as the time to get acclimated managing any side effects associated with the treatment and determining if you can fit this treatment into your life. This is not the time to be wondering if the treatment is working; that will come later. 5. Do not overly focus on those things you can not control 6. Surround yourself with supportive friends, family and health care providers that help you follow these rules and lift you up when you are down. My hope is that this virtual MS Center provides one of the ways for you and your families to follow these rules and adjust to your MS over time. Question: I have secondary progressive MS and have been wheelchair-bound for several years. A few years ago it was discovered that I have blood clots in my legs and I have been on a therapeutic dose of Coumadin ever since. Is this common? Are there any ways to increase blood flow without the use of medication?
Answer: Blood clots in the legs or Deep Venous Thombosis (DVT) is a common complication in anyone with decreased mobility especially those wheelchair bound. Remember, blood is pumped by your heart into arteries that supply oxygenated blood to your limbs and organs but there is no pump except your muscles to return the blood to your heart through your veins. It is the contraction of your muscles that pumps the blood back to your heart much like squeezing toothpaste out the tube. If your muscles do not move the blood sits longer in your veins and can clot. Often the first symptom is swelling of one leg below the level of the clot or pain. One of the reasons graduated pressure stockings are used is to prevent swelling of the legs and the formation of these blood clots. (Click 'read more' below...) Question: I do not have MS but I have (had?) Acute Transverse Myelitis in 1977. It is now 37 years later and I am curious if any of you are seeing TM patients with symptoms simiiar to Post Polio Syndrome? I have been out of work now for 2 years after fairly sudden onset of fatigue, joint pain (mostly knees and hips so below level of injury) and muscle weakness. It is absolutely not just aging out of a skeleton that may have been off kilter for all of these years.
Answer: Acute transverse myelitis (TM) is an inflammatory condition confined to the spinal cord, often associated with a recent viral infection, and often occurring in young individuals like yourself at the age of 19. The hallmark symptoms are acute (hours to a few days) to subacute (1 to 4 weeks) onset and progression of back pain, weakness and sensory loss below the level of spinal cord involvement, and loss of bowel and bladder function. It follows the rule of, “thirds” with 1/3 experiencing near complete recovery, 1/3 partial recovery and 1/3 with little recovery. The condition rarely reoccurs and people rarely develop Multiple Sclerosis. There are alternative conditions to exclude, but this is a straightforward matter in most cases. Depending on the degree of residual problems, it is not uncommon to observe worsening symptoms later in life. The worsening symptoms and function may be related to secondary problems such as the development of arthritis, scoliosis or contractors or may be related to what the questioner referred to as “post-Polio” phenomenon. By this we mean that the nervous system has a limited capacity to compensate for injury and respond to stress; this capacity may be overwhelmed with time and lead to accelerated aging or neurodegeration of pathways that previously were responsible for recovery. All individuals with significant residual symptoms and problems from TM (or any other neurological condition) should undergo periodic reevaluation (at least every few years) by someone with expertise in neurorehabilitation to ensure adequate adaption and recovery ensues and to prevent or manage secondary complications that arise over time. An excellent source of information is The Transverse Myelitis Association (myelitis.org) Rip Kinkel, MD PLEASE NOTE: The information/opinions on this site should be used as an information resource only. This information does not create any patient-HCP relationship, and should not be used as a substitute for professional diagnosis and treatment. Please consult your health care provider before making any healthcare decisions or for guidance about a specific medical condition. 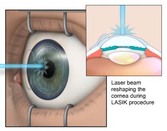 Answer: A person with MS should not be precluded from Lasik surgery (or PRK surgery) simply because they have MS, but I would recommend a thorough Neuro-ophthalmolodical evaluation before this surgery is considered. The most important issues to consider prior to corrective surgery are the following:
The one thing that would not prevent you from having lasik surgery is treatment with any of the disease modifying therapies for MS. The exceptions to this rule would recent treatment with chemotherapy (cyclophosphamide and mitoxantrone) and steroids (solumedrol, methylprednisolone, prednisone); I would recommend being off chemotherapy and steroids for at least 6 months before considering lasik surgery. I would check this advice with the ophthalmologist who will be doing the lasik surgery as well as your neurologist to make sure there are no special considerations in your case. Rip Kinkel, MD PLEASE NOTE: The information/opinions on this site should be used as an information resource only. This information does not create any patient-HCP relationship, and should not be used as a substitute for professional diagnosis and treatment. Please consult your health care provider before making any healthcare decisions or for guidance about a specific medical condition. Question: I originally had vision problems in 2000, along with a normal Visual Evoked Potential (VEP). In 2001 I had my first go around with severe spasticity in both of my legs. By 2003 my 2nd VEP came back abnormal. During these times my brain MRI's as told to me were normal. Due to financial problems, I was unable to have another MRI until 2013. My brain MRI showed white spots, and my neurologist said "those are MS lesions" when she looked at the prints, but when she looked at my MRI on her computer she then said "No, those are pockets of spinal fluid". With my spine MRI the orthopaedist said that "No, they were not of bone matter", and did not know what an MS lesion looked like. My neurologist seems to think they are "bone". My orthopaedist stated I do not have buldging disks, herniated disks and have a very very mild degenerative area in my hip, "but not enough to treat". My neurologist went strictly by the written report of so called "clean MRI" via the radiologist. What do you think?
Answer: It sounds like you’ve gone at least 14 years without a definite diagnosis of MS and even now there are questionable findings on your diagnostic evaluations. Usually, this is very good news and means that even if you do have MS it is a relatively mild form of the disease. Of course there are exceptions to this rule and you should be evaluated by an MS specialist. Amazingly, there are not a lot of trained MS specialists so you may need to check around your area or even travel a ways to find one. It is hard for me to give you any more advice without knowing the specifics of your case. To find a trained MS specialist in this area, click on this link from the National MS Society (NMSS): http://www.nationalmssociety.org/Treating-MS/Comprehensive-Care/Find-an-MS-Care-Provider/Partners-in-MS-Care Good luck and feel free to give us some feedback after seeing an MS specialist.  Approximately 5% of people with MS experience onset of the disease under the age of 16. The diagnostic criteria for adult and pediatric onset MS is identical but the differential diagnosis differs; specifically, children more commonly experience acute disseminated encephalomyelitis (ADEM), a mono phasic form (this means it happens once unlike MS) of inflammatory demyelination most commonly associated with recent viral infections or immunizations. The international pediatric MS consortium has established diagnostic criteria for MS and ADEM to ensure that children with ADEM do not prematurely receive a diagnosis of MS. ADEM can look very similar to MS at first but the children rapidly become quite ill and encephalopathic (meaning confused and lethargic often with behavior changes and sometimes progressing to coma), which is very rare in MS, and the MRI appearance is typically quite different. Unfortunately, 10-20% of children do not recover well from ADEM and some will even go on to develop MS. Other conditions considered quite rare in adults must also be considered in a child presenting with an MS-like disorder, but these conditions are usually easy to exclude by an experienced neurologist with appropriate diagnostic evaluations. There are key features of Pediatric MS that dictate a slightly different therapeutic approach compared to adult onset MS: 1. Kids with MS tend to experience far more inflammatory activity than adults; This means more relapses and more new lesions developing on repeat MRI scans. This also makes it far easier to use relapses and MRI activity to guide therapeutic decisions. In my experience it is important to initiate therapy early in these children, monitor their response closely and alter therapy if they are not responding either by clinical or radiological criteria. 2. While there is no evidence that kids respond differently to disease modifying therapy, they certainly hate injections as much as adults and in my experience require a lot of guidance and supervision to make sure they keep to their treatment schedule. This is particularly true of kids with MS once they leave home to go to college. Newer oral and infused therapies may improve adherence to treatment regimens 3. Kids with MS are often treated with IV immunoglobulin (Ig) for relapses, a practice now rare in adults. I rarely find that IV Ig therapy is as useful as treatment with steroids in kids or adults. If a kid does not respond to high dose steroids for a relapse, I prefer to treat them with plasma exchange 4. Kids with MS often look quite good to the casual observer but cognitive problems occur early and can interfere with learning and school; if unrecognized these cognitive problems may manifest as a behavioral disturbance. Kids with MS do best with learning center evaluations and adaptions that allow them to thrive better in school. This is particularly true when frequent relapses interfere with large chunks of the school year. 5. Kids with MS tend to develop disabilities at a younger age, but it is hoped that early aggressive treatment will change this outcome. 6. Kids with MS do best with support and interaction with other kids with MS; remember they are really a minority and most programs are geared for adults. 7. Lastly, it is important to look after the parents of kids with MS. They are the best resource available to the child but the disease can cause a lot of stress and family disruptions. Supportive group activities for parents, especially those with disabled children, and the ability to get away even for a few hours are highly constructive. It is also best for parents to have direct assess to their doctor for emergencies or concerns. The Pediatric Multiple Sclerosis Alliance is just organizing and would be a great place to start for support. You can click on this link for pediatric MS groups and resources: http://www.healthcarejourney.com/pediatric-multiple-sclerosis.html -Rip Kinkel, MD Two questions came in about CCSVI:
"I would like an opinion on whether you think it is "worth a shot" to try venous angioplasty for chronic cerebrospinal venous insufficiency (CCSVI), especially when you have a progressive form of MS for which there is no other treatment available?" The other was "Why do you think CCSVI only works well the first time" Answer: There has been a lot written about Chronic Cerebrovenous Insufficiency (CCSVI) and MS, including the treatment of this condition with the so called, "liberation procedure”. This has raised the hopes of many patients and initiated a cottage industry of angiographic intervention by physicians with highly questionable motives. After all the procedure makes a lot of money. Let me be blunt and straight to the point:
There is no current reason to pursue either evaluation or treatment of CCSVI unless;
I understand that there are those of you who feel desperate and will try anything for your MS, but this treatment can be harmful. There have even been deaths directly attributed to the “liberation procedure”. Please avoid evaluation or treatment for CCSVI unless the following conditions are met:
Rip Kinkel |
PLEASE NOTE: This information/opinions on this site should be used as an information source only. This information does not create any patient-HCP relationship, and should not be used as a substitute for professional diagnosis and treatment. Please consult your health care provider before making any healthcare decisions or for guidance about a specific medical condition.
Archives
March 2024
Categories
All
|