Welcome to the Virtual MS Center!
Ask any question you want about Multiple Sclerosis and one of our experts will answer it as soon as possible.
|
Here is My Question:
How often do neurologists disagree with radiology reports? Do you recommend second opinion readings of MRIs and how would I go about getting a second reading of MRIs? Thank you. Answer: We disagree often with general radiologists (they read the majority of MRI scans in the country) and less often with neuroradiologists (most radiologists at academic centers are specialized in MRI of the nervous system and are called neuroradiologists). If your physician would like a second opinion about your MRI, he can send us a message. You would then need to get a copy of your MRI on CD and upload the MRI to our site. We provide the report to your physician. This service is available for $50 and not reimbursed by insurance. If you are interested, send us an email at [email protected] Revere (Rip) Kinkel MD Director of the Multiple Sclerosis Program Professor of Clinical Neurosciences University of California San Diego Question:
How safe is it to have contrast with MRI?. After my first attack I had 2 brain and spine MRIs. All were negative but I still had symptoms and then a year later I had a neg MRI. In April it will be more MRIs with contrast? I am worried they have no idea what I have but with yearly MRI with contrast I am worried how safe this is. Answer: This is a very good question. Please refer to my posting from 9/17/15 for the most up to date information on this subject. I think it is best to minimize the use of gadolinium when possible. This can be done once a diagnosis is established by using volumetric imaging with registration of images to simply determine if white spots (T2 lesions) are new or enlarged since the last MRI scan. If these techniques are not used it is difficulty to determine new activity on MR imaging. http://www.healthcarejourney.com/q--a-for-virtual-ms-center/are-gadolinium-contrast-agents-safe Revere (Rip) Kinkel MD Director of the Multiple Sclerosis Program Professor of Clinical Neurosciences University of California San Diego Here is My Question:
Do I really need another MRI? Over past three years I have been followed by specialist and symptoms have been minimal: tingling, heat insensitivity and chronic fatigue for which I take mess. During this time I was also dx'd with optic atrophy from optic neuritis but again symptoms were subacute. I have had 3 Brain mris. First showed 4 nonspecific white matter changes, with second some had disappeared and with third I was told it was possible to count 8, still nonspecific but radiologist still reports as normal MRI. So now I have to have a 4th a year later. Is it worth it? I mean from point of view of expense as well as exposure to contrast- I have also had spine mris which showed nothing. Is there a real chance I could have MS or am I being followed from an excess of caution? Is another MRI the way to go or would you suggest other testing or nothing? I would really welcome your advice as I am feeling very unsure. Answer: I can understand why you are perplexed. For instance, I would never tell a person with MS that they have “8 lesions” and then turn around and say their MRI is normal. It is possible for an MRI to display innumerable non-specific white matter hyperintensities but this would not be supportive of a diagnosis of MS. The ultimate question is why are your physicians obtaining MRI scans on a regular basis. It sounds as if they are not at all certain of the diagnosis. If this is the case, spinal fluid analysis is quite useful. This is done with a procedure called a lumbar puncture or “spinal tap.” If it is felt that your MRI has not shown any significant changes over 3 years (this is a big if), there is little reason to repeat MRIs frequently. My practice is to obtain monitoring MRIs at 6, 18 and 36 months then 5 and 10 years in people with symptoms and findings consistent with MS (such as your residual optic atrophy) but minimal evidence to support an active diagnosis. Clinical re-evaluations are done on a yearly basis and we move up an MRI scan if we believe the disease has become clinically active. I would never treat an individual without stronger evidence to support a diagnosis of MS. Revere (Rip) Kinkel MD Director of the Multiple Sclerosis Program Professor of Clinical Neurosciences University of California San Diego 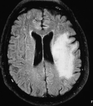 Here is My Question: If my MS is inactive how often do I need to have an MRI? I am claustrophobic and so MRIs are not fun and my doctor says I need one every 5 months? I haven't had any new symptoms so why do I need MRIs so often? Answer: This is a great question. How often a person needs to obtain a repeat MRI really depends on the circumstances. Let’s take the easy extremes to start:
This leaves everyone in between. Current recommendations are to repeat MRIs of the brain only every year unless there is a specific reason to do them sooner; the exceptions include monitoring people with more active disease, monitoring patients in the first year of treatment with a disease modifying therapy and monitoring for the development of PML in high risk patients on Tysabri. Most asymptomatic MS disease activity is reflected by an MRI of the brain so the spinal cord is less important in most circumstances for monitoring. Of course, it is only useful to repeat MRIs to monitor MS if it is done correctly. Sadly this is usually not the case in most clinical setting. For this reason, MRIs tend to be most useful in the first 5 years after a diagnosis, when it is relatively easier to determine if there is anything new. In the near future we will be rolling out a way for people to ensure that useful information is obtained on repeat MRIs. Stay tuned to this site to learn more. As for claustrophobia, I hear you loud and clear. For diagnostic purposes an open MRI will usually suffice but for repeat image analysis closed systems are preferable. Most people do very well with a good dose of lorazepam (1.5 to 2.0 mg) or alprazolam (same dose) about an hour before an MRI. You will need someone to drive you home Good luck Revere (Rip) Kinkel MD Director of the Multiple Sclerosis Program Professor of Clinical Neurosciences University of California San Diego Here is My Question:
Is there a risk using contrast with getting an MRI? Answer: Typical contrast used for MRI is called gadolinium (a paramagnetic agent that comes across as bright on certain MRI sequences). This is usually fairly well tolerated, although there is a small risk for a drug reaction, and kidney injury. The kidney injury is not common, but can occur more frequently in individual with kidney impairment at the time of the gadolinium administration. Most institutions require a recent blood test (creatinine) to check kidney function prior to the MRI. It is also not recommended to receive multiple/frequent gadolinium-enhanced MRIs within a short period of time as this may increase the risk of kidney injury (or gadolinium associated nephrotoxicity). For the typical MS patient, this is not a significant concern. A. Scott Nielsen MD MMSc Virginia Mason Multiple Sclerosis Center Question:
I’ve read that sometimes signs of MS can be “invisible” on an MRI for various reasons: old areas of damage, MRIs performed without following specific “MS Protocols” (size of slices, strength of MRI machine, etc.), abnormalities that are seen diagnosed as normal “due to age,” etc., and that a general neurologist may miss signs that an MS specialist would catch. I ask this because at age 29 I became very, very ill. Up until that time I had remarkable health. Symptoms included vertigo (w/nausea), horrible headaches, extreme weakness and fatigue, difficulty swallowing any food, and excruciating traveling pains throughout my body. When taking a shower, for example, the water hitting my skin felt like shards of glass. My heart would race and I would get chest pains but cardiologists said my heart was fine. I would wake up with horrific muscle spasms, especially common were my hands. My symptoms progressed to where my vision would go dark and I would feel close to fainting. I could not hold my urine. My doctors ruled out Hepatitis, Lupus, HIV, Syphilis, and various other conditions. Ultimately I was diagnosed with Depression/Anxiety/Fibromyalgia/Chronic Fatigue Syndrome. It took 12 years for a doctor to think of ordering a brain CAT scan, results which were reportedly normal. After around 14 years, I was treated for late-stage Lyme disease & associated co-infections (as I did have a bull’s-eye rash in the beginning) by a Lyme specialist. But after ten years of treatment, despite some improvement, my PCP urged me to discontinue treatment. Now, in addition to my typical flare ups, I am experiencing visual problems. Double vision/eye muscle weakness; episodes of eye pain that can last for days and leave me with blurred vision in that eye; and most recently “light shows” - streaks of light in my upper and lower visual field that do not correlate with my headaches. Two ophthalmologists can find nothing wrong within my eyes. But both are baffled as to why they can’t seem to correct my double vision with prism lenses. Last year my son, at age 31, was hit with visual problems, blacking out/near fainting spells, severe vertigo, fatigue and leg weakness. He was taken to the ER and an MRI was immediately done finding “innumerable lesions” throughout his brain. He was diagnosed with MS. Upon hearing this, I asked my PCP & Neurologist for a brain MRI for myself. The results were reported to be “normal for patient’s age,” other than an area that was possibly an inconsequential small arachnoid cyst. So I am wondering, since some are finding MS may “run” in families, could it be possible I have MS, but perhaps my continued symptoms are from nerve damage from old lesions? Or perhaps it is the Lyme flaring up since I have been off those meds? Answer: MRI is a very powerful tool in diagnosing and monitoring disease activity in MS patients. It provides the opportunity to understand the extent of the disease in terms of the number and location of lesions, but also helps us understand the impact of brain loss that occurs as a consequence of disease progression and normal aging. Brain loss can be seen as "black holes” as well as brain atrophy. With standard MRI sequences, brain atrophy is usually not reported as it is difficult to quantify with standard MRI techniques. Brain volume can be quantified with a variety of techniques that are usually done in research studies. As an example, we are conducting a study at the University of Colorado that will longitudinally measure brain volume in MS patients on highly effective therapies and compare with brain volume on healthy controls. This study will allow us to understand the extent of brain volume loss in MS patients and compare with similar individuals without MS that are simply going through the normal aging process. In addition, other MRI techniques, like MTR, allow us to identify pathology (demyelination) in areas of the brain that appear normal to the naked eye. This technique coined the term “normal appearing brain”. This is likely the reason why patients clinically deteriorate, however, MRI might not be able to capture pathology over time. Augusto Miravalle, MD Associate Professor of Neurology Vice Chair, Education Director, Neurology Residency Program Faculty Member, Rocky Mountain MS Center University of Colorado Denver School of Medicine |
PLEASE NOTE: This information/opinions on this site should be used as an information source only. This information does not create any patient-HCP relationship, and should not be used as a substitute for professional diagnosis and treatment. Please consult your health care provider before making any healthcare decisions or for guidance about a specific medical condition.
Archives
June 2024
Categories
All
|