Welcome to the Virtual MS Center!
Ask any question you want about Multiple Sclerosis and one of our experts will answer it as soon as possible.
|
I started rituximab today. How long before I would know if the circulatory B cells have been reduced and by how much?
Your CD19 and CD20 B cell count will be reduced very rapidly after rituximab treatment, but it will not be necessary to recheck your B cell counts for at least 3 to 6 months depending on the dose that you received. Your doctor will explain this to you. Rip Kinkel, MD  Here is My Question: Is there any reason people with MS shouldn't use Rogaine (or Minoxidil), since you are applying a molecule that's changing vascular permeability so close to the brain? Answer: That is a very interesting question. Minoxidil is a vasodilator when given orally that will lower blood pressure. This can occur when given topically but is rare since a much smaller amount of the drug is absorbed through normal skin. It has also been studied as a drug to enhance delivery of chemotherapeutic and biologic agents to brain tumors by enhancing the permeability of the blood brain tumor barrier. This barrier is distinct from the normal blood brain barrier and over expresses ATP sensitive potassium channels, the target of minoxidil for this purpose. I can find no evidence that minoxidil has any significant effect on blood brain barrier permeability in healthy people or those with multiple sclerosis. Furthermore, it would likely have less of an effect when administered topically, since so little is absorbed and that which is absorbed would still go through first pass metabolism in the liver. Rip Kinkel, MD PLEASE NOTE: The information/opinions on this site should be used as an information resource only. This information does not create any patient-HCP relationship, and should not be used as a substitute for professional diagnosis and treatment. Please consult your health care provider before making any healthcare decisions or for guidance about a specific medical condition. 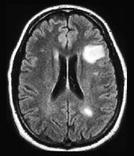 Here is My Question: Dr. Kinkel, After my son's visit today to discuss his latest MRI results, Dr. Q said "No changes but the old lesions are still there and we need to do all we can to keep him stable." Now is this what they call damage? And this is what causes all of my son's issues right? He has numerous old lesions & the one they found on his right frontal lobe is still there..is there a chance some could go away? Answer: Interpreting MRI scans can be confusing to both patients and neurologists, so let me keep this answer as simple as possible without being misleading. Dr Q was likely referring to the “white spots" on the MRI scan when he/she made the statement, “ No changes but the old lesions are still there…..” Think of these white spots as ancient fossil foot prints left behind by dinosaurs. What you can say about these dinosaur fossils holds true for these "white spots” on MRI: 1. The footprints do not mean there are dinosaurs still present nor do the white spots on MRI mean there is still active MS, although neither excludes the possibility of dinosaurs or active MS. Both represent residual evidence of something that occurred in the past. In fact it is very difficult to tell when the white spots on an MRI occurred if you do not have prior MRI scans that show this area of the brain without the white spots. 2. Once these white spots on the MRI are present for several months they do not go away, much like the dinosaur footprints. MS related white spots often get smaller in the months following their formation but it is uncommon for them to completely disappear. This is in contrast to some other diseases where the white spots often do disappear. 3. The underlying brain tissue seen as a white spot on MRI may be functioning almost normally or nearly destroyed. The MRI sequence used to detect the white spot is not able to determine the structural integrity or function of the tissue. Similarly, the ground underneath the dinosaur footprint may be normal (just compressed) or destroyed. Therefore, when you are told that the white spots on an MRI look the same with nothing new, this is a good thing but not the only thing. You also want to know if other features of the MRI suggest ongoing disease activity that may be producing further damage. Some of these other MRI features can be inferred from other imaging sequences (not the sequences that show the white spots) but most require research MRI techniques. In practice our main goal is to make sure that there are no new white spots appearing after we start a treatment for MS. This is one of our main initial goals of therapy. Rip Kinkel, MD Here is My Question:
Have people with MS reported the Nuvigil is significantly more effective than Provigil? Answer: There are no head to head studies and any reports would be anecdotal at best. Rip Kinkel, MD That is a good question, as many people think they are different things but they aren't. MS relapses and exacerbations are synonymous (the same thing). Please refer to this previous blog on the subject...CLICK HERE
Rip Kinkel, MD Here is My Question:
Hi there, I was diagnosed with MS in 2012 and have been symptom free since 1 month ago. Now I am experiencing symptoms again like tingling in my hands and feet. My doctor put me on a oral steroid but I don't think it's working. First, what happened that made the tingling come back and will it go away? Also, do oral steroids really work or should I have just done an IV of SoluMedrol? I have recently started Tecfidera and hoping for good results. Thank you for your time :) Answer: I can understand your concern but rest assured that the temporal pattern of the symptoms that you’ve described since 2012 is quite common. Although I do not know the facts of your individual case, I can make the following general comments:
I hope this answers your questions. You should certainly discuss these concerns with your MS doctor at your earliest convenience. Rip Kinkel, MD PLEASE NOTE: The information/opinions on this site should be used as an information resource only. This information does not create any patient-HCP relationship, and should not be used as a substitute for professional diagnosis and treatment. Please consult your health care provider before making any healthcare decisions or for guidance about a specific medical condition. Here is My Question:
Is there an increased risk of relapse after stopping Rituxan the way there is with Tysabri? Second, does Rituxan preclude patients from taking other drugs such as Tecfidera or even Tysabri and others in the future? Third, does the JCV+ antibody test done with Tysabri also mean a person has that same risk of PML with Rituxan? Answer: These are all very good questions for which we currently have only partial answers.
All of these answers must be tempered with some degree of caution as there here have been limited controlled studies of rituximab treatment in MS patients . For the time being these are the best answers that I can provide based on the evidence available. Rip Kinkel, MD A very large study of Copaxone for primary progressive MS showed no meaningful benefit of treatment compared to placebo. Smaller studies of Copaxone for progressive MS that were done prior to its approval for relapsing MS also failed to show any meaningful benefit of Copaxone in this phase of the disease.
Rip Kinkel, MD Please note that the RSS feeds on our Home Page and the News & Events page are not showing. The website developer is currently working on this. Thank you for your patience.
 This really depends on the part of the back involved; I will confine my response to lower back pain, also called lumbar back pain. In my experience low back pain in MS patients is infrequently a direct effect of Multiple Sclerosis but often a secondary complication of MS. Remember, most of strain on your body from either prolonged sitting or standing is transmitted through the lumbar spine region. This make people in general very susceptible to mechanical low back pain. Patients with MS are specially prone to this type of pain because of abnormal walking patterns, asymmetric truncal weakness, and improper seating support. These are the types of problems best evaluated by a rehabilitation specialists and an adaptive seating and technology specialist. Rip Kinkel, MD Here is My Question:
If a patient develops IRIS after stopping Tysabri, do you recommend the patient resume indefinitely the use of Tysabri even if the JC Virus antibody counts increase to an unsafe level? Answer: There is no simple answer to this question. Everything in medicine requires us (an you) to balance potential benefits of treatments with potential risks. For example, let’s assume that your risk of PML goes up to 1 in 100 because you suddenly have a high JCV antibody index. This is a 1 % risk. Let’s also assume that you were initially JCV antibody negative with a risk of PML estimated at no more than 1 in 10,000 or 0.01% when you started treatment with Tysabri. What you need to ask is what potential benefits are worth this new risk? If I told you that based on your prior history with MS your risk of a relapse within 6 months of stopping Tysabri is 30% and your risk of a severe relapse is 10%, would this make you continue Tysabri therapy despite the increased risk of PML? The answer may be yes, but only you can decide. This new risk may become more acceptable to you if your doctors monitor you closely for early pre symptomatic PML by obtaining MRI scans every 4 months. That is how I view this kind of change in risk; I need a way as a doctor to mitigate this risk. Now, what if your risk of a severe relapse after stopping Tysabri is only 1 to 3 % in the first year? Perhaps you would now decide to switch to another therapy to avoid the risk of PML? The main problem we face is our difficulty gauging a person’s risk of severe relapses after stopping Tysabri. We also find it difficult to gauge a person’s risk of becoming disabled within short time intervals (i.e. 3 to 5 years). Therefore, discussing the potential short term benefits of a therapy is very difficult because of the variable nature of MS. In my opinion the greatest risk of severe relapses after stopping Tysabri is a patient with > 2 relapses in the 2 years (or one relapse in the prior year) before starting Tysabri, a large T2 lesion burden on MRI (this means a whole lot of white spots on your MRI), residual disability from recent relapses before starting tysabri and multiple active (gadolinium enhancing) lesions on an MRI scan obtained at least 6 months after starting the prior disease modifying therapy you were taking before switching to Tysabri. The risk of a relapse after stopping Tysabri is highest with all 4 risk factors and goes down to a minimal risk if all 4 risk factors are absent. However, as I’ve stated previously, it is also my opinion that one should not stop Tysabri unless you plan to start another disease modifying therapy immediately. An individual who develops IRIS after stopping Tysabri is at risk of this happening again, particularly if this occurred while receiving another disease modifying therapy. I would be hesitant to discontinue Tysabri in this circumstance without the guidance of an MS expert who has treated many people with Tysabri. As always, please discuss these complex issues with your neurologist. He or she should be able to help you analyze your specific MS features so as to allow you to make the best decision. -Rip Kinkel MD PLEASE NOTE: The information/opinions on this site should be used as an information resource only. This information does not create any patient-HCP relationship, and should not be used as a substitute for professional diagnosis and treatment. Please consult your health care provider before making any healthcare decisions or for guidance about a specific medical condition. Here is My Question:
How often do you need to have an MRI when on Tysabri? I have been on it for 1.5 years, JCV negative, and MRIs looked unchanged since starting Tysabri. My neurologist wants me to have them once a year, but I feel uncomfortable about that. What's your opinion? Thanks! Answer: The risk of PML remains low because you are repeatedly JCV antibody negative. If your MRI is stable on Tysabri after 1.5 years, your risk of new MS activity is no more than 2%. Therefore, repeating the MRI every year in this circumstance is reasonable, as long as you remain JCV antibody negative. It is far more important that you have your JCV antibodies checked every 6 months at a minimum. Some doctors check every 3 months. If you become JCV antibody positive, you will definitely need more frequent MRI monitoring -Rip Kinkel, MD PLEASE NOTE: The information/opinions on this site should be used as an information resource only. This information does not create any patient-HCP relationship, and should not be used as a substitute for professional diagnosis and treatment. Please consult your health care provider before making any healthcare decisions or for guidance about a specific medical condition.  How do optic neuritis attacks affect the physical shape and appearance of the impacted eye? The way we used to teach medical students about optic neuritis is through the following paraphrased quote from our textbooks, “The patient sees nothing out of the eye and you see nothing abnormal when examining the eye.” What this means is that there is no visible change to the eye. There may be swelling to the optic nerve head when the doctor looks at the retina with his ophthalmoscope, but this is temporary and not externally visible to anyone. --Rip Kinkel, MD IRIS is an acronym for Immune Reconstitution Inflammatory Syndrome. It simply defines the restoration of an inflammatory response against an organ or organs after these normal immune responses were impaired by a disease (e.g.. HIV) or a drug (e.g.. Tysabri). This response is neither organ or disease specific; it is most commonly observed after immunodeficient HIV positive patients are given highly active retroviral treatment with a rapid reconstitution of normal immune responses.
The IRIS response may be in response to an ongoing infection like PML or may simply represent the aggravated return of an immune mediated condition like MS or thyroiditis that was suppressed by either the disease or the drug. The existence of this syndrome following discontinuation of Tysabri is somewhat controversial as many authorities believe this is just a bad relapse; nevertheless, the outcome is still the same. Think of IRIS in the following manner; while a patient is on Tysabri the immune response against the brain of MS patients is prevented from entering the nervous system. When you stop Tysabri, if this immune response is still active and the brain is receptive, inflammation can return to the nervous system in a manner analogous to a dam breaking and flooding the valley below. This usually occurs 4 to 6 months after stopping tysabri, when the effects have washed out. This response is not inevitable (less than 10% of patients experience this response) but if it has occurred in the past in an individual patient it is more likely to reoccur when Tysabri is discontinued again. -Rip Kinkel, MD PLEASE NOTE: The information/opinions on this site should be used as an information resource only. This information does not create any patient-HCP relationship, and should not be used as a substitute for professional diagnosis and treatment. Please consult your health care provider before making any healthcare decisions or for guidance about a specific medical condition. Question:
Some studies (mostly molecular) give hints that melatonin could be beneficial for oxidative damage and protection of mitochondria, and therefore perhaps beneficial for MS. Are there any side effects of melatonin that should prevent us from taking it? Thanks! Answer: Thanks for your question on the use of melatonin to prevent oxidative damage in MS. We asked Dr. Dennis Bourdette, Chair of the Department of Neurology at Oregon Health & Science University to comment on this, as he is an expert on the subject. Here is his response: While there is some evidence that melatonin may have anti-oxidant effects and anti-oxidants may be beneficial for MS, melatonin can have side-effects if taken improperly. Melatonin has an important biologic role in setting our brain's internal clock and in particular in modulating our sleep-wake cycle. Melatonin levels rise about the time we normally go to sleep and causes drowsiness. For this reason, taking melatonin at bedtime can help some people who have difficulty falling asleep. It may also help to re-set one's internal biologic clock when traveling to different time zones, i.e. help in overcoming "jet lag" and helping "shift workers." Melatonin has also been used to help treat seasonal affective disorder by taking it in the evening and using light therapy in the morning. Taking melatonin at times of day other than one's usual bedtime runs that risk of altering one's normal sleep rhythm and may cause daytime drowsiness. I therefore strongly recommend not taking melatonin except at bedtime and really one should only be using it to help with sleep induction in people with sleep disturbance. Dennis Bourdette, MD, FANA, FAAN Chair and Roy and Eulalia Swank Family Research Professor Department of Neurology School of Medicine PLEASE NOTE: The information/opinions on this site should be used as an information resource only. This information does not create any patient-HCP relationship, and should not be used as a substitute for professional diagnosis and treatment. Please consult your health care provider before making any healthcare decisions or for guidance about a specific medical condition.  Here is My Question: I haven't had feeling in my feet in over 9 years. Why is it that I get horrible foot cramps that clench my muscles up for several painful minutes when I do something as simple as apply pressure to a certain part of my upper thigh or even scratch an itch in my lower back?! Am I weird? Answer: You are not weird at all. Foot cramps and spasms can be caused my abnormal reflexes in your spinal cord that create spasms in the muscles of your feet (common in MS) or irritability of the muscles on the bottom of your feet (arch muscles) often spreading to your big toe. Foot cramps are very common even in people without MS. These can and often do occur even when an individual has no sensation in their feet. This is because the parts of your nervous system responsible for sensation (peripheral nerves and sensory pathways in the spinal cord) are separate from those areas responsible for cramping and spasms (muscles and motor pathways). There are many causes and many treatments of cramps and spasms, so contact your doctor to get evaluated and find a solution. -Rip Kinkel, MD Here is My Question: My daughter has been on Tysabri for almost 4 1/2 years. At the end of year 2 she was put on "holiday" and after 3 months had what seemed to be a relapse but was in fact declared IRIS. She received steroids and was immediately put back on Tysabri. At the time, she was told that she could never come off Tysabri. Fast forward 2 1/2 years. Her JC virus antibody values have tripled in the past nine months and are now at 1.3. This would suggest coming off Tysabri but what about the IRIS? Answer: The risk of PML on Tysabri is related to duration of therapy over two years, JCV antibody index and whether or not a patient has received prior immunosupression. For my response I will assume your daughter has not been treated with an immunosuppressant in the past. According to our current understanding of these risk factors (CLICK HERE to read my previous blog on Tysabri risk), your daughter’s current risk of PML is approximately 1 in 1,000 or 0.1%. This number is taken from the figure below showing the risk of PML after 2 years of Tysabri therapy according to various JCV index levels. We have no information at present to suggest that the manner in which JCV antibody index values vary over time affects the risk of PML. The risk stratification is based on current index value and current duration of therapy. I hope this helps with your decisions. -Rip Kinkel, MD
PLEASE NOTE: The information/opinions on this site should be used as an information resource only. This information does not create any patient-HCP relationship, and should not be used as a substitute for professional diagnosis and treatment. Please consult your health care provider before making any healthcare decisions or for guidance about a specific medical condition.  Here is a blog that was written about Vitamin D...CLICK HERE Here is a video about Vitamin D as well...CLICK HERE Also, please go to the search box at the top right side of this page and type in Vitamin D, as there is quite a lot about it on this website. -Rip Kinkel, MD Do You Know About High Dose Cyclophosphamide For Immunosuppression Without Stem Cell Rescue?5/8/2014
Question: Is there somewhere to read about patients' personal experiences about receiving high dose cyclophosphamide for immunosuppression without stem cell rescue? All I'm able to find is medical articles which are not that enlightening to someone looking to get a the treatment who doesn't know anything about medical terms. Thanks!
Answer: Unfortunately, there is nowhere I know of to read about patient experiences for this. So, I will open it up to people with MS who are reading this who might be able to provide some insight. -Rip Kinkel, MD |
PLEASE NOTE: This information/opinions on this site should be used as an information source only. This information does not create any patient-HCP relationship, and should not be used as a substitute for professional diagnosis and treatment. Please consult your health care provider before making any healthcare decisions or for guidance about a specific medical condition.
Archives
June 2024
Categories
All
|