Welcome to the Virtual MS Center!
Ask any question you want about Multiple Sclerosis and one of our experts will answer it as soon as possible.
|
Here is My Question:
I've noticed that my ESR number from my yearly physicals has gone down over the past few years, from a high of 43 in 2010 to now at 21. Does this mean anything? Answer: The ESR or sedimentation rate is a non specific acute phase reactant. The value will go up with infections and any chronic systemic inflammation. It also tends to go up with age. Values fluctuate from one test to another within the range you mention without being significant. In my experience this test is not very useful in MS patients and should not cause you any concern. Revere (Rip) Kinkel MD Director of the Multiple Sclerosis Program Professor of Clinical Neurosciences University of California San Diego Question:
I read an interview with Dr. Richard K. Burt who is performing HSCT at Northwestern. He mentions this treatment is most promising for people with RRMS but that there are other forms of stem cell therapy that hold great promise for people with progressive MS. Do you know anything about these therapies? Answer: Please read some of the postings on our website concerning stem cell transplantation for MS. There are several stem cell trials underway that involve progressive MS patients but none have reported any results. Prior small studies in this population of patients have not demonstrated any significant benefit. Revere (Rip) Kinkel MD Director of the Multiple Sclerosis Program Professor of Clinical Neurosciences University of California San Diego Question:
Hi my question is regarding MRI reports. I have seen the term "volume loss in the brain" multiple times when obtaining a copy of the MRI report, but my doctor has never mentioned this as an issue to me. Should I be concerned? Answer: The term, “volume loss”, on an MRI report is usually accompanied by the phrase, “greater than expected for age.” As you may know, we gradually lose brain tissue volume as part of the normal aging process. Certain diseases of the nervous system, such as MS, accelerate this volume loss. Even in the most benign cases of MS, we usually notice greater volume loss than expected for age after years of disease. Few neurologists pay attention to this volume loss for several reasons: 1. Until recently there was no way to accurately measure this brain volume loss except in research studies or even determine if the amount of volume loss per interval of time (say a year) was greater than expected. Soon these techniques will be available in clinical practice. 2. We know of no therapies that halt this volume loss, although certain highly active therapies such as alemtuzumab (Lemtrada) and ocrelizumab (not available yet) slow down this loss of volume to near normal rates. 3. Most MS therapies are approved based on clinical trials that used relapse rates and the development of new T2 hyperintensities (the white spots on MRI) as the chief outcome measures. Therefore, most neurologists in clinical practice primarily use these outcome measures to determine if a drug is working. Studies over the past 25 years have demonstrated that the brain is able to compensate for loss of brain tissue, in individuals with significant passive and active neuronal reserve (see prior blogs on this subject). Briefly, passive reserve refers to the amount of enrichment and education you receive during development and active reserve refers to ongoing mental and physical stimulation and learning through adulthood and old age. Therefore, the mere presence of volume loss should not concern you now. Continued volume loss, on the other hand, at rates greater than expected is associated with the development of both cognitive and physical disability. Therefore, it is increasingly important to measure this MRI metric to determine if your treatment is working adequately. This is particularly important in people who are over 50 or with longstanding MS, since they rarely have relapses or noticeable new MRI T2 lesions even when a treatment is not working adequately. In these individuals it is perhaps not accurate to say that everything is stable merely because these measure remain stable. Stay tuned for more information on this important topic. Revere (Rip) Kinkel MD Director of the Multiple Sclerosis Program Professor of Clinical Neurosciences University of California San Diego Question:
Hi! I am a 49 year old male and 3 years ago I was tested for MS. I had a weird episode that lasted a month. Started like alot of MS patients with numbness and tingling and tremors mostly on my right side. I felt electric shock down spine and then all resolved. Went to emergency room and saw MS specialist and he did lots of tests. All blood work fine and MRI fine. He said there was low possibility of MS. For 3 years I have walked with my legs feeling like bricks as muscles feel like I have done a huge work out. I have a hard time occasionally swallowing large foods. I'm very tired and numbness comes and goes. My brain feels weird...only thing I can describe is it is like I had some attack that effected my brain. My GP after and year and half did only Brain MRI and again it was normal? Fast forward 2 years later and I still have the same symptoms other then I had pain in right eye for a long time. Now it feels like it's very sensitive to touch and feels like something is behind it. So Do I have MS? Am I crazy thinking maybe it's older onset to MS? Is there anything close to MS that we need to look at? We did a Lyme Disease test and vitamin b12 and lupus 3 years ago and all good. I live in Canada and it takes forever to see a specialist. Thank you for reading this story. Answer: You probably do not have MS. Normal repeat imaging after 3 years of symptoms makes this diagnosis unlikely. You should be evaluated at least one more time by an experienced neurologist. This is far more important than any repeat testing. Most of our diagnoses are based on a careful, detailed history and examination. Keep an open mind to the possibilities and a good neurologist should be able to help. Good luck. Revere (Rip) Kinkel MD Director of the Multiple Sclerosis Program Professor of Clinical Neurosciences University of California San Diego Question:
I'm looking for a doctor who specializes in MS depression, anxiety, and cognitive issues Answer: Many MS specialists are very experienced at the management of these particular problems; other MS centers collaborate with neuropsychologists, psychologists, social workers and psychiatrists to help manage depression, anxiety and cognitive issues. You may want to contact the local National MS Society to learn if there are specialists in your area that can help with these concerns. There are also resources to find specialists listed on our depression and anxiety symptom page READ MORE Revere (Rip) Kinkel MD Director of the Multiple Sclerosis Program Professor of Clinical Neurosciences University of California San Diego Here is My Question:
My daughter is on Tysabri for MS in Australia but she seems to have had relapse, her white blood cells are higher than they should be, will she be able to continue with this medication? Answer: Thanks for the question. Elevated white blood cells are common when using Tysabri. By virtue of how this medication works, a process of "demargination" occurs where white blood cells no longer cross the blood brain barrier and do not stick to the blood vessel wall (leading to an excess of circulating white blood cells). This is normal. Determining the effectiveness of Tysabri for a given patient is something your daughter's neurologist can help with. Some considerations for your doctor will be 1) how long has the Tyasbri been used, 2) are the symptoms indicative of a confirmed relapse (some symptoms may not be an actual relapse), and 3) what was the MS disease course prior to starting the therapy. Since I do not know your daughter's situation, I cannot comment on the usefulness of Tysabri in her case. However, I have had patients that need a little more time on the medication before the disease gets under better control. I would encourage you to attend the clinic visit with your daughter if able and discuss with the neurologist. A. Scott Nielsen MD MMSc Neurologist and MS Specialist at Kaiser Permanente Use the search box in the upper right on this page and type in "Tysabri" to learn more about Tysabri.  Hey everyone! Mindy Eisenberg's new book, Adaptive Yoga Moves Any Body, just came out! Mindy's book is a guide for all ages and abilities with clear instructions and hundreds of photos. Ideal for:
Mindy has been kind enough to give away copies of her book, so register now! Three winners will be selected on Friday, February 12th. We will announce and contact the winners then! Register below to win! Here is My Question:
Can MS start late in life? I am experiencing hand dexterity issues. Answer: MS can certainly start late in life, although this is uncommon. Problems with hand dexterity in the elderly or even middle aged adult can be caused by a multitude of different problems. I am not sure why you are concerned about MS, based on the information provided, but a good neurologist should be able to figure out the reason for your problem. Revere (Rip) Kinkel MD Director of the Multiple Sclerosis Program Professor of Clinical Neurosciences University of California San Diego  Hey everyone, We get lots of questions about which diet to follow if you have MS. Tad Campbell, MCN, RD, LD is a registered dietitian at the University of Texas Southwestern Medical Center’s Total Life Care (TLC) MS clinic and also serves as the Education Coordinator for the Clinical Nutrition department in UT Southwestern’s School of Health Professions. CHECK out his tips below for eating to reduce inflammation. How many of these are you doing for the New Year???
You can download and print the PDF with all these tips below:
Here is My Question:
I am claustrophobic and scared of MRI's. I have been through an MRI with intervals of 10 minutes inside and 2 minutes out, through the whole hour I went through this process. They can put me to sleep but not fully. What can I expect by not being fully asleep?? Seems my claustrophobia is getting worse. Answer: Claustrophobia and MRI imaging doesn't mix very well. Aside from the intense anxiety, movement of the patient within the scanner makes the images very difficult to interpret. The institution that can put you "not fully" asleep, is likely using a form of conscious sedation. For individuals with severe claustrophobia, this is a good option. What this entails is usually oral medication you would take before the scan that would essentially cause you to sleep (or at a minimum, not care that you are in a scanner). There are different protocols base on the institution you are at (and the specifics should be discussed with them). Regardless of the protocol, you should make sure you have a ride home as you will not be capable of driving for a while! A. Scott Nielsen MD MMSc Neurologists and MS Specialist at Kaiser Permanente Here is My Question:
I was wondering if anyone could comment on the risk of Autism or ADHD associated with children born to Mothers with MS. I have heard a medical professional say there is an association, but I am curious to know your thoughts. Thank you!! Answer: There are mixed studies on this topic. Some studies have found an increased risk of any developmental disorder (including autism and aspergers) in children of mothers with one of many autoimmune disorders (not just MS). Others have found no relationship. Some studies have seen an association when there are any family members with autoimmune disorders (not just the mother). In general, when studies have found an increased risk, they have been quite low. More research is needed on this as the mechanism (if an association exists) remains unclear. Benjamin M. Greenberg, MD, MHS Director, Transverse Myelitis, Neuromyelitis Optica Programs Director, Neurosciences Clinical Research Center Co-Director, Pediatric CONQUER Program UT Southwestern Medical Center Childrens Health Dallas, Texas Question:
I was diagnosed in january 2012 with an attack of optic neuritis. They classified my MS as inactve. All my lesions in my brain were not active and I have been told that I have had it for years. Can they classify it as inactive after a first official attack?? I have not had any flares since then, only symptoms worsened due to stress or heat but went away by using a short course of steroids. Thank you. Answer: Activity is defined by the presence of definite new MRI lesions or definite relapses in the prior year. Therefore, based on your history it is appropriate to term you inactive since January 2013. Revere (Rip) Kinkel MD Director of the Multiple Sclerosis Program Professor of Clinical Neurosciences University of California San Diego Question:
What are the signs of PML? Answer: PML causes subacutely progressively (developing over weeks) neurological symptoms and findings that can be quite similar to an MS relapse. Some common symptoms of PML that are less often observed in MS included large visual field deficits and language deficits. PML does not create spinal cord problems so a “relapse” confined to the spinal cord (which is common in MS) is unlikely to be caused by PML. Revere (Rip) Kinkel MD Director of the Multiple Sclerosis Program Professor of Clinical Neurosciences University of California San Diego Question:
When you test for MS and then first MRI is normal and then a year later it is still normal, when should you do another MRI? I'm continuing to have symptoms such as stiffness, fatigue, eye pain, numbness and tingling. Answer: The answer to your question really depends on the likelihood that you have MS. For instance, if you experienced a clinically isolated syndrome (optic neuritis is an example) and your MRI is normal at onset your chance of developing MS over the next 10 years is less than 20 %. Repeating an MRI scan one year later is reasonable but if the repeat scan is normal, I would wait another 2 years before scanning again. Of course, if definite new symptoms consistent with MS occur during this follow-up interval, I would repeat the MRI earlier. People with signs and symptoms that are less specific for MS (examples include fatigue, stiffness, tingling without exam findings) do not require multiple repeated MRI scans; repeating an MRI one year later is probably sufficient unless definite symptoms and signs of MS appear. Revere (Rip) Kinkel MD Director of the Multiple Sclerosis Program Professor of Clinical Neurosciences University of California San Diego Here is My Question:
Is there a study on Aubagio and its side effect of depression? I am using Aubagio now for 40 days and I feel no side effect other than deep depression. Is it related to the new medication? Answer: I'm sorry to hear about your difficulty with depression. Unfortunately, ~50% of patient with MS will struggle with depression at some point during the course of their illness. I am not aware of a specific association between Aubagio and depression (we do see an association with interferon-beta therapies). I searched the prescriber brochure, clinicaltrials.gov, and searched the medical literature, but could not find a reported assocation between Aubagio and depression. You can learn more about the association of depression and multiple sclerosis here (http://www.healthcarejourney.com/depression-and-anxiety.html) I'd advise that you speak to your PCP and neurologist (or psychiatrist if you have one) regarding your symptoms. A. Scott Nielsen MD MMSc Neurologist and MS Specialist at Kaiser Permanente 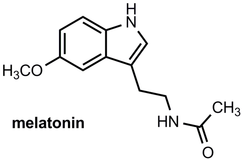 Here is My Question: How much Melatonin can be safely taken at night? Answer: Melatonin is not regulated by the FDA even though it is a hormone. There are potential side effects but usually with doses much higher than those readily available. Studies suggest that melatonin is NOT a good sleeping pill compared to any of the available sleeping pills on the market. There are studies indicating that melatonin is useful for resetting your circadian rhythm to restore normal sleep patterns. This is typically a problem with shift work, jet lag or people who have either accidentally or on purpose reset their biological clock and no longer are able to go to bed at the usual time. For people with normal sleep patterns, the pineal gland begins secreting melatonin at around 9 pm and this progressively make you more sleepy. Therefore, most of us recommend 3 mg of Melatonin at 9 pm in order to go to sleep by 11 pm. Once your circadian rhythm is reset Melatonin will have no further affect and should not be needed anymore. MS patients have lots of reasons for disrupted sleep, all of which require different treatments. To know how to treat these different sleep problems requires an adequate history and sometimes additional testing. Revere (Rip) Kinkel MD Director of the Multiple Sclerosis Program Professor of Clinical Neurosciences University of California San Diego #melatonin Here is My Question:
Does Difen Flex contain Cortisone? Answer: I do not believe there are any steroids in Difen. This is a strong, non steroidal antiinflammatory agent (NSAIA) like ibuprofen. The word “Flex” may mean there is a muscle relaxant combined with the NSAIA. Since this drug is not available in the United States, I am not sure of the actual ingredients. Revere (Rip) Kinkel MD Director of the Multiple Sclerosis Program Professor of Clinical Neurosciences University of California San Diego Here is My Question:
How long does Plegridy stay in your system after you stop taking it? Answer: Plegridy is excreted through the kidneys. If an individual has kidney disease that can affect the speed at which plegridy is washed out. A recent article published in the Journal of Clinical Pharmacology (see link) looked at the pharmacokinetics of plegridy in patients with various degrees of kidney impairment and healthy patients. Their data indicate that after an injection of plegridy, the detection of the drug in the blood stream was below the lower limits of detection (ie, 1.3 nanograms per milliliter) by day 14. http://www.ncbi.nlm.nih.gov/pmc/articles/PMC4303928/pdf/jcph0055-0179.pdf A. Scott Nielsen MD MMSc Neurologist and MS Specialist at Kaiser Permanente Here is My Question:
I was on Tysabri for 5.5 years until testing positive for JC antibodies. My neurologist took me off everything for three months so I could start Tecfidera, his concern being that he wanted me totally Tysabri-free before introducing another MS drug. During the detox my condition worsened. I've now been on Tecfidera for 25 months and my EDSS score has climbed from 5 to 6.5. My neurologist referred me to another neurologist with more experience with MS drugs and he gave me the option to remain on Tecfidera or go back on Tysabri. I should mention that while on Tysabri my condition remained largely unchanged--it's only since getting off that I've gone downhill. The new doc says that at the October 2015 European MS conference there was a roundtable discussion where it came out that after two years off Tysabri the immune system resets itself with regard to Tysabri and PML risk. He thinks Tysabri is a viable alternative for me and, should I choose it, I will only need to detox from Tecfiera for 30 days. His thinking is to only be on Tysabri for two years or less given the promise of drugs in the development pipeline, though he did say we'll have to play it by ear. Unfortunately, there doesn't seem to be many numbers for someone that far out of Tysabri yet. So, I'd like to know more about the numbers before committing, however. That's where you come in. I have a great deal of respect for how you seem to have your hands around the numbers, something I've never come across before. My neurologist has given me a script for blood work (to be taken in the next couple months) and it seems to make sense to have it taken at the end of my 30 day detox to get an accurate pre-Tysabri number rather than now. I'd like to go ahead with the Tysabri and would like to stop Tecfidera in the middle of January. I'd like to get an updated JC antibody titer then too. The only one I have is from 2.4 years ago. Unfortunately, most of my cell counts from Labcorp are only displayed as a number within a reference range or percentages. There aren't any absolute numbers of CD8 cells like other people have reported. Hell, I don't see CD8 cells listed. Is it possible to convert my numbers to what other people report? Wait, my absolute lymphocytes are 1100 and lymphocytes are 17%, and both are listed as within the normal range. So, my questions to you are 1) what do I have to ask Labcorp for to get the numbers everyone else seems to be using? 2) When I get a JC anitbody titer in February, what number should I hope for to feel good about my odds back on Tysabri?, and 3) what do you think about someone with my history going back on Tysabri? Answer: You’ve asked some very good questions, so let’s see if I can answer each one. 1. I am not aware of any cases of PML starting more than 6 months after stopping Tysabri. Those who develop PML during this interval likely had asymptomatic PML, even before the Tysabri is stopped. Therefore, it does not take anything close to 2 years to “reset” the immune system after stopping Tysabri. This process occurs within 3-6 months of stopping Tysabri. 2. The problem with stopping Tysabri and waiting several months before starting another DMT is the high risk of MS relapse within 3 to 6 months of stopping Tysabri, as you found out the hard way. For this reason, most MS specialist do NOT use a “wash out” period in any patient switching from Tysabri to another DMT. I do obtain an MRI before stopping Tysabri to evaluate for possible PML. If the MRI shows new T2 hyperintensities, especially those associated with Diffusion weighted Trace image signal, I make sure there is no evidence of PML before restarting either Tysabri or another DMT. 3. For those patients who are great candidates for Tysabri and responding well to treatment, many of us increase the interval between Tysabri infusions to every 2 months (56 days) if the patient becomes JCV antibody positive 12 months or greater after starting treatment. This is particular true of older (> 50) and thinner (less than 60 kg) patients. We then usually monitor for PML with brief MR scans every 4 months (a 7 minute scan with FLAIR and DWI trace images only without gadolinium). There is increasing evidence that dosing Tysabri in this manner dramatically reduces the risk of PML. 4.For patients on tecfidera with normal lymphocyte counts (like yourself), I see no reason to wait a month before starting another DMT. Remember, the only known risk factor for PML in Tecfidera treated patients is an absolute lymphocyte count less than 600. I would simply obtain an MRI of the brain before stopping Tecfidera to make sure everything is stable. In your case, Tysabri is a reasonable choice. I would restart on monthly Tysabri infusions with repeat MRI of the brain every 6 months. The infusions should be extended to every 2 months (56 days) after 12 infusions with more frequent MR imaging of the brain. Alternatively, your MD could consider treatment with Ocrelizumab when this becomes available. This will hopefully occur by the end of 2016 Good luck Revere (Rip) Kinkel MD Director of the Multiple Sclerosis Program Professor of Clinical Neurosciences University of California San Diego |
PLEASE NOTE: This information/opinions on this site should be used as an information source only. This information does not create any patient-HCP relationship, and should not be used as a substitute for professional diagnosis and treatment. Please consult your health care provider before making any healthcare decisions or for guidance about a specific medical condition.
Archives
June 2024
Categories
All
|
||||||