 Recent changes in the healthcare system and medical advancements offer the hope of more effective management of complex chronic diseases such as Multiple Sclerosis; but many patients and providers are undeniably frustrated by the day to day reality of these changes, whether it be the need to switch insurance plans and providers, the larger copays and deductibles, the increased requirements for prior authorizations, the increased documentation requirements to receive payment, the shorter times available for visits and the never ending announcements of the next cure or advancement that arrives too late or not at all. Now that we have all expressed our frustration and got it out of systems, I’m here to tell you it is time to stop complaining and focus on managing those things we can control. Change is always hard and we need to find constructive ways to manage change and harness the benefits of common advancements like the electronic medical record (EMR) systems required under the Affordable Care Act, better known as Obamacare. Let’s start with how to maximize the benefits of a typical doctor-patient visit. For years I’ve watched people arrive for their visits unprepared. A doctor arriving unprepared is also common, but since your only recourse is to get rid of the doctor, let’s focus on the patient side of the equation. How many times have I listened and tried to understand the chronology and characteristics of a patient’s problem in the privacy of the exam room while they discuss and sometimes argued with various relatives or friends about the facts of their case? I have a secret for you; these interactions between patients and those who accompany them are often more instructive to the doctor than the medical facts, but I digress. People spend a great deal of time keeping their resume and financial records up to date but how many actually keep their medical records up to date. When I ask a patient for discrete information like the start and stop date of a prescribed medication or a hospitalization their answers are often incorrect by years. I know what you’re thinking because I’ve heard it from my own family members; many of you believe that because the doctor or nurse or some other health care professional is writing everything down that all of your history and data is carefully preserved and shared among all providers. Well it isn’t. Many also believe that medical institutions share records and results. Perhaps in the future, this will be the case, but at present we are limited by an extensive series of privacy laws called the Health Insurance Portability and Privacy Act of 1996 (HIPAA). As with most regulations, HIPAA is a great idea at face value but the funding to comply with HIPAA is not available and information flow actually is slower under HIPAA because of the security requirements and medico legal concerns. So the bottom line is that even if your health information is carefully recorded (a big if) it is not shared easily or willingly. And even if it was carefully recorded it is your responsibility to make sure the information is accurate and available for appointments. So the main step you must take to get the most out of your interactions with the health care system is to take control and responsibility for your own health information. Even the best electronic medical system may crash on the day of your visit, so you might as well have a back up ready. I am going to outline the main things you and your doctors need to do to improve visits. In subsequent blogs and additions to this web site we will implement and provide some of these features for you; then you can decide with whom you want to share your medical information at any time by a simple click of a button. All that is required is a computer and Internet access. A scanner is useful for document storage. Once information is inputted either a smartphone or tablet app can be created to provide ongoing or updated information. 1. If your health care provider uses an electronic medical record (EMR) system use it to its full potential. Ask to review the information already entered and make corrections as necessary. This is something useful to do while waiting for the doctor and is actually your right under the HIPAA regulations. Reviewing your information is a necessary step since doctors often repeat information in your chart to save time and perpetuate mistakes. For instance, I had a patient that was admitted years ago for abdominal pain eventually diagnosed with severe viral gastroenteritis after discharge. The doctors were worried about pancreatitis on admission but never removed this diagnosis from his record. All subsequent notes list this man as having a past medical history of pancreatitis. Most electronic medical record systems also allow you to communicate with your doctor and his facility through a secure Internet portal. At Beth Israel Deaconess Medical Center this was called patientsite and on Epic based systems like UCSD this is called MyChart. This gives you access to almost all your medical information and sometimes gives you access to your doctors’ notes. You can ask questions, see results of testing and copy it for your records, and refill medications and schedule appointments through these systems without waiting on telephone hold. If these systems are available to you, sign up and use them. But remember, if you are seeing doctors at two different institutions, their EMRs will not communicate yet and may not for a long time. This is one advantage of staying within one system. In the future a system of Accountable Care Organizations (ACO) will formally create networks of health systems that shares your medical information and are accountable for your care. The different ACOs will not necessarily communicate with one another but communication among the health systems within each ACO will be improved. 2. You need to keep a medical history on your computer and bring a print out or your computer or tablet to visits. If you’ve completed step 1 above, then this will not be necessary once you establish care with a doctor who uses an EMR system. The average MS patient sees a new doctor every 3 years so it is best to be prepared for these new interactions. Hopefully, this information will not be required after your initial visit with your new doctor, but it is better to be safe than sorry. Just as there are templates for resumes online, there are many templates for personal medical histories as well. We will be posting a medical history form for MS patients soon and provide a secure online site to update this information 3. Keep copies of test results in a notebook or better yet, scan them into your health record on your computer. Make sure the file name identifies the scanned document. For instance an MRI report could be assigned a file name, MRI_Brain_3.13.14, to indicate an MRI of the brain on March 13th, 2014. Remember, if a test is done at your doctor’s facility it will appear on his EMR system, but if you do it closer to home or in another facility, chances are your doctor will never see the results unless you make sure he or she gets them. Think of this when you are in a hurry to leave after an appointment and decide to skip the blood draw lab and get tested closer to home. It becomes your responsibility to make sure somebody actually sees the result. 4. Medications are a special part of your health record. Federal requirements for certain payments to doctors require health care providers to use EMRs to prescribe and record medications electronically. Gone are the days of doctors scribbling illegible prescriptions on paper pads and handing them to patients. The only exception is controlled substances, which still cannot be sent electronically; this includes narcotics (vicodin, Percocet, Darvocet morphine etc), benzodiazepines (diazepam, lorazepam etc) and stimulants (methylphenidate, Adderall etc). Different states have slightly different requirements for controlled substance prescriptions. If you have a doctor who uses an EMR, never leave without a corrected and updated list of your medications for your records. Whenever you start or stop a medication you should add these dates to your medical history (# 2) with the reason for starting or stopping the medication clearly stated. If you are seeing a doctor for the first time and do not have a list of your medications, the next best thing is to bring all the bottles of your medications to your appointment. 5. MRIs are a very special part of your medical record and one that is often not available when needed at the time of a visit. MRIs help establish or confirm your diagnosis and form the basis of many treatment decisions. Unfortunately, insurers sometimes require that you obtain an MRI outside of your doctor’s institution or you end up choosing another MRI facility because is more convenient or less expensive or both. There are two problems with this system. First, these outside MRIs will usually not be available to your doctor unless you bring an electronic copy on a CD. When the MRI facility tells you they will send a copy to your doctor, they are lying. The only thing they will send is a useless report. They may say they will send a CD but this rarely occurs. Make sure you do not leave without a CD of your MRI in your hands to take to you doctor or to upload for your doctor (see below). The second problem is that an outside facility may not perform the type of MRI needed for your situation even if asked. It is my opinion that all Brain MRIs on MS patients should be acquired using both 3D FLAIR and 3D T1 sequences but these are rarely done in practice. In the near future it will be important for you and your doctor to make sure that the MRI facility is willing to do the correct image acquisition before agreeing to let the facility do your MRI. Why is this important? Soon you will be able to take your MRI on a CD or directly from the radiology center and upload it to a CLOUD server that will perform quantitative analysis that allows your doctor to make more accurate and timely treatment decisions. Stay tuned as we will be posting access to one of these servers on this website in the near future. 6. Now it is time to talk about the actual visit with your health care provider; you’re all prepared and probably nervous. Broadly speaking there are 3 types of patients I encounter; those doing their best to convince me that they have serious problems and want help, those trying to perform at their best to convince me that everything is all right so as to get a good report and those somewhere in the middle. Each type of patient require a different approach but, as with politics, it is usually best to remain somewhere in the middle. By this I mean it is important to analyze information carefully, recognize both the positive and the negative during your visits and take a measured approach focused on achievable goals. How do you get there?
Remember, more accurate and readily available information can only improve the quality of your healthcare. -Rip Kinkel, MD
2 Comments
 Exercise is probably the most important therapy for MS and serves as the platform for all other treatment modalities.
This being said, some people have difficulty initiating and continuing exercise programs for reasons both related and unrelated to their MS. Since the perceived barriers to exercise are almost too numerous to list, I find it far easier to list some core principles to follow:
I am often asked a variation on the same question, so I thought it best to write a blog that addresses the entire concept. The question is often phrased in one of the following ways:
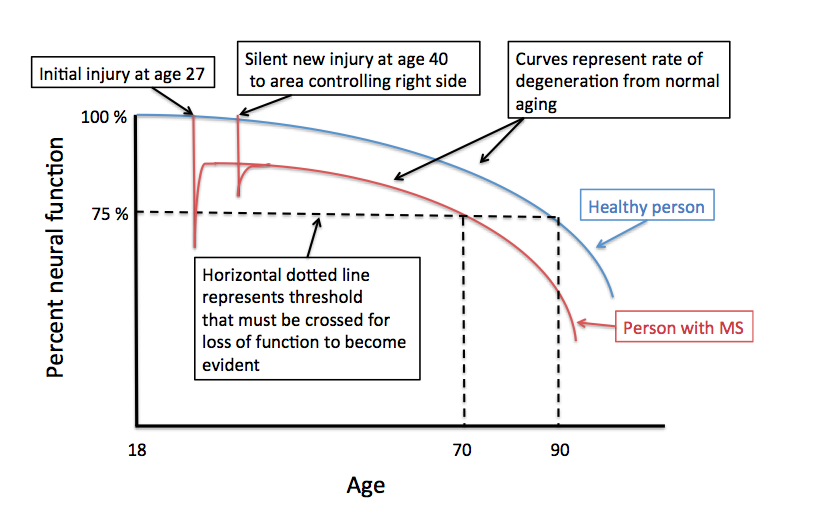
The theme of each question is identical; why after years of stability would someone with MS slowly get worse? There are, of course, several possibilities; it is most important for an individual with this concern to consult with an MS specialist or neurologist to determine the most likely reason for this delayed worsening after many decades of stability. One common cause is that the person has developed a new problem unrelated to MS, such as cervical spondylosis; this is a form of arthritis that can cause compression of the spinal cord with progressive walking difficulties often with stiffness and limited range of motion in the neck and neck pain that migrates into one or both arms. Many other reasons for delayed onset of neurological symptoms in an MS patient exist and require an evaluation to sort out. Another possibility is that the individual is developing secondary progressive MS; in some MS Clinics when this occurs after a single attack, the MS course is referred to as, “single attack onset progressive MS”. Determining if this is the cause of the worsening can be difficult and often requires years of observation for the clinician to be sure. More commonly, a person develops secondary progressive disease after experiencing more typical relapsing remitting MS earlier in life. The years of relatively stability without relapses before the onset of progressive worsening is not unusual, as relapses tend to get rare as you get older. The real question is what is happening during those years or even decades of stability? To answer this question in a manner that is easier to visualize I created the figure to go along with this blog. The Y-axis represents percent neural function and the X-axis is age. The figure begins at age 18 after the conclusion of normal development; at this time you should have 100% neural function assuming no injuries during development and adequate enrichment (diet, exercise, education, nurturing). The blue curve represents the gradual decline in neural function with age. This decline is probably not linear and is certainly affected by many life events as well as illnesses and chronic diseases.
Eventually, a normal healthy individual crosses a certain threshold of declining neural function, represented by the horizontal dashed line, and is no longer able to compensate well. In the example provided this occurs after the age of 90. I’ve labeled the threshold as 75% of normal neural function, but this is an arbitrary percentage; the threshold may be lower or higher or variable by region depending on a number of factors including physical and cognitive enrichment during development and ongoing physical, cognitive and social activity throughout adult life. We refer to these factors as passive and active neuronal reserve, respectively. Most studies indicate that active neuronal reserves, or your physical, cognitive and social activities in adulthood, are the most important in determining the affects of normal aging and the outcome from chronic neurologic disease like MS. The red curve represents a theoretical MS patient who experiences their first neurological symptoms at the age of 27; let’s say this causes left sided weakness. At the time of this attack (or exacerbation) the area of the nervous system responsible for the left sided weakness is temporarily injured and neural function declines below the 75 % threshold. This causes the patient to experience the behavioral manifestation of this decline in neural function (e.g. left sided weakness). In the example provided complete recovery of this behavioral manifestation of the neural injury (the left sided weakness) occurs even though the area is no longer able to provide the same level of neural function as a normal individual (i.e. the red line does not return to the blue line). This recovery occurs because of partial injury at onset, resolution of inflammation, remyelination and repair and neural plasticity (other areas of the brain taking over the behavioral function of the injured area or new connections forming from the injured area or both). In this same example the patient is remarkably stable and does not experience any further injury from MS until the age of 40. This time the injury does not cross the threshold and no symptoms occur, even though the area involved normally controls right-sided strength. An MRI may or may not show a new area of involvement and tissue recovery occurs once again. As we now trace out the red line while the person ages, we notice that the line crosses the 75 % threshold at an earlier age (age 70) than the healthy person represented by the blue line (age 90). At this age the MS patient can expect their left sided weakness to return and they will now slowly develop new right-sided weakness from the prior silent injury at the age of 40. How can this be prevented? One way is to prevent further injury from MS by using effective disease modifying therapies. The best way to shift the threshold line lower and therefore prevent the onset of declining neural function with age is to increase your active neuronal reserve. This is done by remaining healthy and actively involved with life through regular physical exercise, cognitive activity -particularly learning new skills- and remaining engaged socially. Now you know why I continually harp on the importance of remaining active in all these domains of life. Rip Kinkel, MD |
DISCLAIMER:
The medical information and opinions on this site are provided as an information resource only, and are not to be used or relied on for any diagnostic or treatment purposes. The information and opinions expressed do not create any patient-physician relationship, and should not be used as a substitute for professional diagnosis and treatment. Please consult your health care provider before making any healthcare decisions or for guidance about a specific medical condition. Archives
January 2020
Categories
All
|
- Home
- About Us
- Virtual MS Center
- News & Resources
- Seminar Registration
- Health & Wellness
- Blogs
- About MS
-
Symptoms
- Balance and Walking Issues
- Breathing/Respiratory
- Bowel Dysfunction
- Cognitive Dysfunction
- Crying/Laughing Uncontrollably (PBA)
- Depression and Anxiety
- Dizziness/Vertigo
- Dysphagia
- Fatigue
- Foot Drop
- Hearing or Smell or Taste Changes
- Heat Sensitivity
- Leg Weakness
- Loss of Hand Dexterity and Coordination
- Memory and Mutliple Sclerosis
- Migraines
- Numbness/Tingling/Altered Sensation
- Nystagmus and Oscillopsia
- Pain
- Sexual Dysfunction
- Sleep Issues
- Spasticity/Spasms/Cramps
- Speech/Swallowing
- Urination/Bowel Problems
- Vision
- MS Clinics
- MS Topics
- Register With Us
- Terms of Use/Privacy/HIPAA
- MS HealthCare Journey

 RSS Feed
RSS Feed
