 I am often asked to provide advice on diets, vitamin supplementation or other complimentary approaches to the management of MS. While there may or may not be a role for some alternative approaches to MS management, I find that patients are often putting the proverbial ’ Cart ahead of the horse’, when they ask these questions. The question that should be asked is, how do I remain active, independent, socially engaged, and overall mentally and physically healthy with this disease? This is no small task given the barriers and challenges faced by MS patients. Some in the neurological community believe these goals can only be achieved with so called disease modifying therapies of which the older injectable therapies are usually regarded as the platform therapy on which all other treatments are built. While it is true that these pharmacologic disease modifying therapies have a significant role to play in MS disease management, I have a different idea of what represents a platform therapy. To me platform therapies represent those management strategies, often adjustments in lifestyle and health behavior, that will prevent the development of or modify those other medical conditions (known as co-morbid conditions) known to have a detrimental physical and mental effect on MS patients. So what are these health behaviors and co-morbid medical conditions? I think you know the answer but I will list them anyway (in no particular order): 1. Smoking 2. Obesity 3. Type II Diabetes Mellitus 4. Hypertension 5. Osteoporosis 6. Low vitamin D levels 7. Depression, anxiety and chronic daily stressors Every one of these health behaviors or conditions has been shown to have a detrimental effect on MS outcomes. More importantly, some of these risk factors interact with one another in a synergist manner, meaning that their combined effects are worse than their individual effects. So what is my platform therapy prescription? It involves 5 crucial steps: First, focus on improving your mental health; without modification of chronic symptoms of depression and anxiety, modification of common chronic stressors harmful to your MS and your health, and continued social interaction and participation, other therapies will fall short in achieving their goal. This can be a tall order. You will lay the foundation for this goal by stopping unhealthy behaviors, exercising regularly, eating well and taking care of other health concerns (see below). But this is often just the starting point. Now is the time to consider a closer examination of lifestyles, relationships, and career or work issues. While it can be difficult to find a therapist, either group or individual, that works for you, it is well worth the effort. Often online support groups now form the basis of support for many patients. Some patients will require medications as well but rarely in isolation. Most importantly, it is time to consider what is important and what is not important in your life in order to help in this process. But remember this is a lifelong process; do no be discouraged and always keep working to achieve peace and happiness. Second, stop harmful health behaviors, notably smoking. Although alcohol consumption in moderate amounts has not been linked to more rapid progression of MS, alcohol abuse and other illicit forms of drug use, particularly cocaine and narcotics, are in my experience associated with worse outcomes.. Third, build a pattern of behaviors that is likely to achieve ideal body weight and maintain activity levels. This is extraordinarily difficult for many and often a lifelong struggle. I am not a big advocate of a particular diet; in fact it seems that the best results occur with increased activity level associated with a reduction in calories and a change in diet. Over the years, many of my patients have reported feeling better and losing more weight after switching to gluten free or gluten light diets. While there is no evidence that this diet specifically alters the course of MS, it certainly seems to have indirect benefits. In those patients morbidly obese (usually defined as 100 lbs over ideal body weight) despite efforts to reduce their weight, I am a strong advocate of bariatric surgery, although the safest and most appropriate bariatric procedure will require consultation with your physician and a qualified bariatric center. Increased activity levels are possible in everyone although some patients experience more barriers in achieving this goal, whether as a result of disability, lack of resources or social isolation. Ideally, I want all of my patients to perform aerobic exercise a minimum of 20 minutes a day, 5 days a week. I advise patients to start slow and low and increase gradually, if necessary. A personal fitness instructor or a physical therapist can help you design a program that meets your needs and your physician can advice you on any particular restrictions you may need to follow. Additional strategies must include progressive resistance training (basically weight lifting) to improve and maximize muscle function. Again a personal fitness instructor or a physical therapist can help you design an appropriate and safe program. Lastly, many patients report benefits in flexibility, strength and physical and mental well being as a result of group or individual yoga programs. Fourth, supplement your diet with vitamin D3; the evidence is clear that low vitamin D3 levels are associated with the risk of developing MS and MS disease activity after onset. Whether vitamin D supplementation modifies the course of the disease remains unclear until larger studies are completed. Supplementation with 5,000 to 10,000 IU a day is safe in the vast majority of patients and should achieve your goal of obtaining a 25 hydroxyvitamin D level over 50, if not closer to 100. Fifth, focus on modifying co-morbid health states like hypertension, osteoporosis and diabetes if these conditions are present. All too often patients neglect their other physical and mental health concerns after a diagnosis of MS, either as a result of feeling overwhelmed or helpless to achieve the desire results of therapy because of the barriers imposed by their combined conditions. This is a mistake. Hypertension, osteoporosis and diabetes are all associated with a more rapid rate of MS progression. Diabetes in particular creates a number of management issues in MS patients and makes the disease more difficult to treat. Dr. Kinkel This blog was originally posted in 2013. We are organizing the site and in order to move the blog we had to re-post it. Our apologies to those that have already read it.
0 Comments
 So you’ve been told that you may have Multiple Sclerosis (MS). To borrow a common phrase, this is likely “freaking you out” and creating a great deal of anxiety. Take a breath, get comfortable and start reading. Rule 1: MS is rarely fatal and it is very rare for MS to cause disability in the first few years after diagnosis. You have time to get the medical opinions you need to make decisions and determine if anything else should be done to evaluate or treat your condition. This does not mean you should have to wait months to see a doctor specializing in this condition; months perhaps spent worrying unnecessarily. If you have an unnecessarily long wait to see a specialist ask your primary doctor for another referral. Rule 2: An important thing to know is that multiple sclerosis is often difficult to diagnose. Why? Well, there is no one test or exam that can definitively tell whether or not you have MS (nope, not even an MRI). Even after all tests and exams are done, some people cannot be diagnosed for years after the beginning of symptoms. The diagnosis of MS is based on symptoms and examination findings supplemented by diagnostic testing. The process of establishing a diagnosis is inherently complex requiring, at a minimum, the consultative services of a neurologist. A radiologist CAN NOT DIAGNOSE MS based on an MRI scan alone. A radiology report of an abnormal MRI scan indicating possible MS is often a cause of confusion, frustration and undue anxiety. The clinical criteria used to establish a diagnosis may sound complex but are really quite simple; a specialist needs to uncover specific symptoms or findings on examination that indicate inflammation in different parts of your central nervous system (i.e. the brain and spinal cord only) that occurred at different points in time. Very importantly, he or she must exclude alternative diseases capable of presenting in this fashion. Laboratory tests such as MRI scans, blood tests, spinal fluid analysis, and evoked potentials, supplement the clinical criteria and play a major role in confirming the diagnosis and eliminating alternative diagnostic possibilities. Of all these tests, the most important is an MRI scan but this alone can not be used to diagnose MS and must be interpreted by experts with caution. The common radiology report mentioning, “non-specific white matter changes” or “ white matter changes” consistent with MS means nothing by itself. The changes observed on the MRI scans of people with MS are very specific and can be classified for their specificity. For this you will require interpretation by an expert; unfortunately, most radiologists are not aware of this diagnostic criteria. Rule 3: Current diagnostic criteria for MS, revised in 2010, allow the diagnosis to be made at the onset of symptoms in certain people. Most people will need to be followed and obtain repeat MRI scans and clinical evaluations after the onset of their symptoms to determine if they have MS. In most cases the diagnosis can be established within 2 years. Those in whom it is more difficult to establish a diagnosis within 2 years tend to have a more benign prognosis. Rule 4: Certain syndromes (a syndrome is a collection of symptoms and findings developing in a typical pattern over time) are so commonly associated with MS that this diagnosis is strongly considered whenever the syndrome is observed in a person between the ages of 13 to 50. Often these syndromes have names attached to them, such as Optic Neuritis or Transverse Myelitis while others are referred to by less notable and less specific monikers such as Acute Brainstem Syndrome. Newly diagnosed MS cases over the age of 50, and very rarely under13, are certainly seen in our clinics but require a greater deal of care to exclude other conditions (e.g. strokes, degenerative diseases, leukodystrophies). Prior to the era of MR imaging, it was impossible to determine who would go on to develop typical MS and who would be found to have another diagnosis or never experience further neurological symptoms. Patients were considered, “At risk to develop MS” after experiencing typical symptoms for the first time, but were often not informed of this risk since the probability of MS was uncertain, and no therapies were available to reduce this risk or alter the future course of the disease. It took, on average, 5-years to establish a certain diagnosis of MS, a period of significant uncertainty and anxiety for many patients. MR imaging of the cranium and spinal cord, revolutionized this diagnostic process. First, MR imaging allowed clinicians to exclude many alternative conditions that mimic MS and respond best to appropriate therapies initiated as early as possible. Second, MR imaging now allows clinicians to establish a relative risk for the development of MS. For instance, over 50 % of patients have typical MS appearing MRI findings at the time of their first symptoms. The number and location of these abnormalities are strongly associated with the short-term risk of developing a clinical diagnosis of MS. Those individuals with highly typical findings are now considered at “high risk” to develop MS or given a diagnosis of MS immediately. Alternatively, those individuals without typical white matter abnormalities, especially those individuals with normal cerebrospinal fluid studies, are considered at low risk to develop MS with a 5 year diagnosis rate of less than 10 %. Therefore, imaging abnormalities at the onset of MS symptoms can be used to educate and counsel patients appropriately, and make decisions regarding early initiation of disease specific therapy. Rule 5: A definite diagnosis of MS does NOT mean a future marked by disability or loss of the ability to participate in the activities you love and find fulfilling. More than 25 % of people with MS never experience any significant disability without any treatment to alter the course of the disease. Those who require treatment experience significant reductions in symptomatic recurrences; it is increasing common for people to remain without significant disability for up to 3 decades or longer. Rule 6: Despite our current ability to establish a diagnosis of MS earlier and with greater certainty in many people, there are still cases where the diagnosis remains uncertain even with extensive testing. In these cases, the diagnosis should not be made prematurely; rather patients should be educated and counseled about diagnostic uncertainty from the onset. Education and follow-up plans, including repeat MR imaging studies every 6 to 12 months should be established. Repeat MR imaging will determine if characteristic white matter abnormalities have developed in the absence of new symptoms. Those people who experience continued difficulty coping with an uncertain diagnosis, even after appropriate education, may benefit from counseling to help ease the anxieties often associated with this process. Extra Credit: While establishing a diagnosis is beyond the scope of this discussion, it is useful to mention two common diagnostic errors. The first is diagnosing MS in patients with no definable neurological disease. The example provided in rule 1 is typical of this error. It is quite common for MS experts to see patients who have been diagnosed with MS by primary care physicians or other neurologists because of non-specific symptoms, such as general weakness, fatigue or tingling, at times supplemented by “minimal” changes on the MRI. By far the most common syndrome in this group of patients is recurrent parenthesis (i.e. usually described as pins and needles tingling sensations) in the extremities without any discernable abnormalities on neurological exam or diagnostic testing. The condition is so frequent that we often characterize the syndrome as "benign paresthesias". Often the sensory symptoms are accompanied by a history of chronic fatigue and/or chronic diffuse pain suggesting an overlap with fibromyalgia and chronic fatigue syndrome. Rarely, do these people develop MS; more importantly, a premature or inaccurate diagnosis of MS often interferes with the effective management of their condition. The second type of diagnostic error is incorrectly diagnosing MS in a patient who has some other neurological disease. The widespread use of MR imaging has helped to eliminate many of these diagnostic errors but they still occur, often as a result of misinterpretation of MR imaging findings or hasty diagnostic decisions made by a neurologist pressed for time. This type of error can be avoided by obtaining a second opinion with an MS Specialist and making sure you doctor reconsiders the diagnosis over time if unusual signs or symptoms should emerge. -Dr. Kinkel
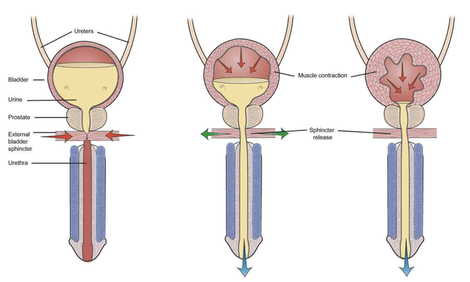
 At the end of the day, people really want to know what is causing their symptoms and how to manage them. Whether you have definite MS or not, there will always be some degree of uncertainty; uncertainty regarding your risk of MS, uncertainty regarding the risk of future relapses, uncertainty regarding the risk of developing disability and uncertainty regarding your response to therapy, whether it be a drug, a dietary change or a lifestyle change. How you and your physician manage these uncertainties together over time defines the art of the doctor-patient relationship. If this process doesn’t work for you with your current doctor, discuss it openly with him or her and, if necessary, find a new doctor. Try to figure out what it is you require from a doctor to help you manage your chronic condition. As in the rest of life there will always be compromises you have to make but try to decide what you find to be most essential. Practical issues such as insurance coverage and distance from the doctor’s office are certainly important when it comes to narrowing down the list of doctors to consider, but should not be the basis of your decision. To me a doctor must first take the time to listen and understand your narrative (doctors call this the “chief complaint”), ask probing questions, explain their interpretation of the information gathered to gain further feedback and information and then put together a plan of action that you are capable of understanding and that clearly addresses your initial complaints. This is much harder than it sounds since often the person describing the “complaint”, is not only unaware of the cause but also unaware of the influence of seemingly random or apparently unimportant aspects of their life on this complaint. To give an example, I am often asked by patients to help them with their daytime fatigue, probably the most common symptom of MS. Many patients simply assume they only need a medication for this complaint and have learned that other patients take various medications for their fatigue. In fact, the causes of fatigue are extremely difficult to unravel and require a skilled history and dedicated follow-up evaluations after testing, activity adjustments and possible medication intervention to arrive at a satisfactory solution. As with most problems in medicine this is an iterative process: First, the complaint is identified and understood as best as possible generating a hypothesis that involves further testing or an intervention; second, the patient is educated about the intervention and given the means to carry out the intervention and track the progress; third, the patient is re-evaluated to determine the initial outcome to the intervention and generate further hypotheses leading to further testing or interventions; etc. This process requires skill, time, empathy and interactive resources. Anyone with a chronic condition wants to find not only a good doctor but a doctor with the support staff and associated medical professionals dedicated to working together on finding individualized solutions to problems. Here is a link to the NMSS to find a qualified specialist in your area: http://www.nationalmssociety.org/Treating-MS/Comprehensive-Care/Find-an-MS-Care-Provider/Partners-in-MS-Care In subsequent blogs we will be discussing these issues at length. I will always begin with the importance of education. Simply knowing the facts, or what is not known, is sometimes all that is needed. Where there are choices to be made I will try to outline them clearly, although it may become clear that I have a bias to express. Remember, an unbiased interpretation of data does not exist. What is important is whether the interpretation of the data is consistent with the known facts and your belief system. -Dr. Kinkel This blog was originally posted in August 2013. We are organizing the site and in order to move the blog we had to repost it. I’ve always enjoyed the “Idiots Guide” series of books and wouldn’t be surprised if there were already one available on bladder function. My intention today is to provide a brief introduction of how your bladder is supposed to work and what often goes wrong in MS. I stole the above diagram off the Internet for purposes of discussion. For woman in the audience, just remove the prostate and the penis and everything else is about the same.
1. Normal bladder function: The bladder is a hollow muscle (called the detrusor muscle) under autonomic nervous system control. This means that it is not directly under your conscious control like the muscles in your legs or arms. Urine flows from the kidneys (not shown) and down the ureters, which are the tubes connecting the kidney and the bladder. Normally, as the bladder fills with urine (left sided picture), the autonomic nervous system (parasympathetic type for those interested in details) prevents the bladder muscle (called the detrusor muscle) from contracting to squeeze out the urine and maintains a lower pressure in the bladder compared to the urethra. The urethra, by the way, is the tube through which urine flows out of you, preferably into the toilet. The pressure in this urethra is kept high by constant contraction of the external urinary sphincter and pelvic floor muscles. This prevents your urine from leaking or emptying spontaneously [note that there is also an internal urinary sphincter not shown in this picture that is also involved in urinary control but we can skip this for the basic discussion. In the diagram above the internal sphincter is located above the prostate in the bladder neck]. When you develop the urge to urinate, there is simultaneous contraction of the bladder detrusor muscle and relaxation the external urinary sphincter allowing urine to flow out smoothly. This coordinated activity is organized in a part of your brain called the pons (part of the brainstem). 2. Failure to store urine (detrusor over activity): This is probably the most common type of problem in people with MS. When MS involves the spinal cord, the detrusor muscle may become overactive. This is because of nerve fibers in the wall of the bladder that sense the stretching of the bladder as it fills, which stimulate neurons in the lower part of the spinal cord through a reflex to cause the bladder muscle to contract. You notice this as symptoms of early filling, urgency, frequency and incontinence when severe. The typical treatment is the use of a class of drugs called anti-muscarinic agents. These drugs work on the parasympathetic nervous system and prevent reflex contraction of the bladder. Common drugs used for this purpose include tolteridone (Detrol), oxybutynin (Ditropan), solifenicin (Vesicare), trospium (Sanctura), darifenacin (Enablex), fesoterodine (Toviaz). There are pros and cons to each of these drugs but all can cause a dry mouth, constipation and less commonly visual blurring. A new drug called Mirabegron (Myrbetriq), is a beta-3 adrenergic agonist that directly inhibits the signals being sent from the bladder to the spinal cord and allows the bladder to fill without contracting. Because it has a different mechanism of action from the anti-muscarinic drugs, we can use it in combination with these drugs in difficult to treat patients. 3. Failure to store and failure to empty (detrusor sphincter dysynergia or DSD): This is probably the second most common problem in MS patients. Imagine your bladder is a balloon filled with air and the opening in the balloon is your urinary sphincter. DSD occurs when there is no coordinated opening of the balloon to let out the air as you squeeze on the balloon with your other hand. In the case of your bladder you experience symptoms such as hesitancy and a poor urinary stream. You may also experience a feeling of not emptying completely (you are correct by the way) and a need to double void, meaning you think you are done but as soon as you get off the toilet or start to leave the bathroom you realize you still need to urinate more. Now your bladder does not have the same elastic properties of a balloon and people with DSD often leave a significant amount of urine in the bladder after they pee because the pressure in the bladder drops below the pressure in the urethra before you empty the bladder. This problem (failure to empty urine) is combined with the problem described previously (failure to store urine) to create urinary frequency, urgency, hesitancy, retention and the need to get up multiple times at night to pee. You may also experience various amounts of incontinence, depending on the severity of your problem, and frequent urinary tract infections because of the failure to flush urine out of the bladder (urine is a great culture medium for bacteria). Treatment involves managing the detrusor over activity with the drugs mentioned above (the anti-muscarinic agents) and trying to relax the urinary sphincter with a different set of medications that often don’t work very well. The medications for the dyregulated urinary sphincter (DSD) include drugs like tamsulosin (Flomax), doxazocin (Cardura) and terazocin (Hytrin). They should sound familiar to most middle-aged men since they are primarily use for prostatic enlargement, which causes similar symptoms. Anti-spasticity medications like baclofen and tizanidine are also sometimes used to treat DSD with variable success. Unfortunately, medications often do not work well for DSD and many people with MS continue to retain urine and experience incontinence and disrupted daily activities from frequent trips to the bathroom. If the amount of urine retained in the bladder is consistently over 100 cc, many physicians will advise intermittent self-catheterization. I usually recommend this only in patients with significantly disrupted lives, frequent incontinence or frequent urinary tract infections. For those with continued problems despite the strategies listed above, there are a number of newer therapeutic approaches that work well including intra-vesicular injection (meaning injection into the internal bladder wall through a procedure called cystoscopy) of Botox, a procedure done quickly in the urologists outpatient office every 3-6 months, neuromodulation with the InterStim® device and various surgical procedures that can often be performed with minimally invasive techniques. These procedures do require specialty management with a urologist. 4. Failure to Empty Urine: This is actually a rare isolated problem in MS and only seen with severe destruction of the lower spinal cord and sacral nerve roots. More often this occurs temporarily because of medication side effect or after a surgical procedure. This problem can only be solved with intermittent self-catheterization since the bladder wall is not able to contract and empty urine. So there you have it; the basics of bladder function and the problems that occur in MS. In future posts we will discuss practical issues such as the pros and cons of different type of catheters, how to avoid chronic Foley catheters, and how to stay dry. Stay tuned... Dr. Kinkel  There has been a lot of chatter and excitement this month about the potential benefits of high dose statin therapy in Secondary Progressive MS. Jeremy Chataway and colleagues reported this month in the online edition of Lancet (March 2014) that high dose statin therapy (Simvastatin 80 mg orally once a day) reduced the rate of whole brain atrophy by 43% over 2 years with benefits observed during both the first and second year of the study. Brain Atrophy was chosen as the primary outcome in this study. This means that changes in the size or volume of the entire brain as measured on MRI scans at yearly intervals were used to determine if there was a difference between the 70 patients treated with Simvastatin and the 70 patients treated with placebo. This outcome was justified based on prior studies showing a relationship between the development of brain atrophy and the development of worsening disability in MS patients. By using brain atrophy as the primary outcome the study investigators were able to observe a treatment effect of simvastatin with fewer study patients and a shorter study time interval. In contrast a study to determine if simvastatin reduced the development of sustained disability in MS would require many hundreds of patients potentially for a longer interval. Interestingly, the investigators did report a possible benefit on two clinical disability measures at 2 years, though the significance of this benefit is unclear at this time. These are very hopeful preliminary results but caution must be advised until further studies are completed for the following reasons:
So what should you do with these results if you have secondary progressive MS? After all, the simvastatin was well tolerated in this group of patients. I suggest talking it over with your physician and certainly consider this drug and dosing schedule if you require statin therapy to lower cholesterol or if you have other accepted cardiovascular or cerebrovascular risk factors known to be benefited by statin therapy. I would also encourage you to participate in any Phase III trials of statin therapy that you may hear about in the coming months Value based medicine has become a recurring theme of health care reform for the past 5 years. The reasons are quite simple. In all developed countries, spending on health care increases in direct proportion to GDP but improvements in health outcomes tend to plateau as spending on health care exceeds 10% of GDP. Think about this as our health care expenditures approach 18% of GDP in the United States; if this statement is true then approximately 1.2 trillion dollars in health care spending per year is not achieving desired outcomes or at worst is wasteful, unnecessary or fraudulent.
So we return to the question, how do we define value in medicine? The corollary to this statement is, when does a procedure or treatment or other billable medical act warrant the costs of that act? Costs in the scenario could be defined as dollar costs, costs from adverse effects or lost quality of life for some interval of time. For decades doctors have argued that patients did not have the training or information to determine quality and value in medicine. This paternalistic and condescending approach to decision making in medicine will continue to fall apart as long as you, the patients, remained engaged in the process. There are many things that can be said about President Obama, but his Affordable Care and Portability Act did create a new agency called the Patient Centered Outcome Research Institute (PCORI) that is tasked with involving patients in the process of determining value in medicine. So it is time for all of you to think about what it means to achieve value in your MS care; you’ve lived it and know the good and the bad of what we have to offer. So let’s hear your thoughts on this topic. What is of value to you in your current care and what would be of greater value to you that is not currently available. Let me give you some ideas to respond to in your replies: Do you value luxurious medical office suites or are the basics okay with certain features like friendly knowledgeable staff and WiFi while you wait? Do you value being able to see or contact your doctor or health care provider when you have a problem or concern? Do you value a doctor who takes the time to explain things to you? What is the minimally acceptable time for an appt with your MS doctor ? 10, 20, 30, 40 minutes? Do you value transparency in insurance coverage prior to signing up? For instance, are you able to find out if an insurance plan covers MRI scans or all the treatments you may be interested in receiving before you sign up for the plan? Would you not value the development of a blood test that could predict your likelihood of responding to a treatment? Would you value greater practical advice from your doctors and health care providers on services they often do not learn enough about in the course of their training such as basics in ambulatory aids, wheelchair seating, diet, exercise and complementary and alternative care? Do you value preventing relapses or preventing disability? Or is your overall goal maintaining or improving quality of life? Do you value the health care journey website where you can go for free to get expert advice and answers to important MS related questions? What would increase the value of the site for you. Just some things for you all to think about as we try to improve the value of medicine through this web site. -Dr. Kinkel  Please go to http://ticnetwork.org/live-stream/2012-convention-coverage/ and click on the "Mission Possible" link for March 18th to listen to the TIC Network interview Christine Granfield, founder of HealthCare Journey. TIC is an award winning radio reading service that broadcasts the reading of printed materials. Until now, they have focused on the blind, but since many people with MS having vision problems, this is a great service for MS patients.  A growing number of our MS clients reside in rental properties, very often the result of the current housing market combined with the financial burden of living with this condition. Although the American Disabilities Act was implemented a number of years ago it has been difficult to enforce. Hence, many rentals are not fully accessible. Many landlords are very accommodating, but some are a bit reluctant to make the necessary modifications to their property for many obvious reasons. The owners of these properties have to look at the costs of the modifications and also possible tenant turnover after these changes have been made. With many of the advances in product design and technology these problems can be overcome. For a large portion of the daily hurdles that an MS client runs up against, equipment has been invented and devised to overcome these obstacles. It is a matter of recognizing the issues and consulting professionals that are versed in this area. These are just a number of simple products that come to mind, for example: Threshold Ramps: Entrance to the home is step one. Aluminum and rubber ramps are available, the best one for your home will be determined by the height of the step and /or door sill. If it's only a 1" rise sometimes a thick door matt with double sided tape to secure it will suffice. See ezaccess.com or pvi.com Floor To Ceiling Transfer Poles: This allows a person to get from 'sit to stand' easier, assuming their upper extremity strength is sufficient and they can transfer safely. The beauty of this item is that it can be strategically placed next to a bed, chair, or a toilet to assist the client, with little or no effect on the property. See healthcraftproducts.com or medline.com Non Permanent Support Rails: many are made for the bed, tub, and toilet areas. There are clamp on, suction, and bed frame mounted rail systems. Again with no damage to the property. Double Door Hinges: Very often a inch or two of doorway clearance can be the difference between accessing a room or not when using a mobility device, especially bathrooms. These hinges allow the door to swing behind the door buck gaining as much as 2 to 3 inches in added clearance. This is an inexpensive way to widen a doorway without removing the door or construction. See Home Depot, Lowes or pattersonmedical.com These are just a few examples of items that are available. Please work with your local PT, OT, and ATP to determine your specific needs. Some of these items are covered by insurances and/or can be written off your taxes as a medical expense if prescribed. Fight On, Big Love.....Tom Mellor ATP To make things easier for you, we are listing new posts in one location. Please visit our "News and Events" page each day (you could bookmark it!) to see what has been newly posted on HealthCare Journey (see link below). Thanks so much for visiting the site!
http://www.healthcarejourney.com/news--events.html |
DISCLAIMER:
The medical information and opinions on this site are provided as an information resource only, and are not to be used or relied on for any diagnostic or treatment purposes. The information and opinions expressed do not create any patient-physician relationship, and should not be used as a substitute for professional diagnosis and treatment. Please consult your health care provider before making any healthcare decisions or for guidance about a specific medical condition. Archives
January 2020
Categories
All
|
- Home
- About Us
- Virtual MS Center
- News & Resources
- Seminar Registration
- Health & Wellness
- Blogs
- About MS
-
Symptoms
- Balance and Walking Issues
- Breathing/Respiratory
- Bowel Dysfunction
- Cognitive Dysfunction
- Crying/Laughing Uncontrollably (PBA)
- Depression and Anxiety
- Dizziness/Vertigo
- Dysphagia
- Fatigue
- Foot Drop
- Hearing or Smell or Taste Changes
- Heat Sensitivity
- Leg Weakness
- Loss of Hand Dexterity and Coordination
- Memory and Mutliple Sclerosis
- Migraines
- Numbness/Tingling/Altered Sensation
- Nystagmus and Oscillopsia
- Pain
- Sexual Dysfunction
- Sleep Issues
- Spasticity/Spasms/Cramps
- Speech/Swallowing
- Urination/Bowel Problems
- Vision
- MS Clinics
- MS Topics
- Register With Us
- Terms of Use/Privacy/HIPAA
- MS HealthCare Journey

 RSS Feed
RSS Feed
