|
Is it just me or is everyone experiencing more difficulty getting treatments approved by insurance companies since the provisions of the affordable care act (Obamacare) went into full force? This seems to be particularly true for patients enrolling in the new and expanded Medicaid plans offered by states (we call it Medi-Cal in California). Let me know your experience with insurance denials of treatment even if the denial was eventually overturned after your physician or their staff provided more information to the insurance company. Take a look at the survey below and let us know what your experience has been:
https://www.surveymonkey.com/s/6FQPC6V Once we have enough responses collected from the survey we will share the information and results with you via this blog. Please note that these surveys are anonymous. Your feedback is appreciated. --Dr. Kinkel Dear MS Community: Six months ago we began this website to provide a one stop, internet information resource for people with MS and their families. We established three rules from the onset; first, all voices and opinions are welcome but readers must know something about the provider and patient bloggers to provide a context for the opinions expressed. Second, no single company or entity would be allowed to dominate the site with their information, as so often happens with pharmaceutical company sites or non-profit sites. Third, we would never sell your contact information to a vendor or a company. We recently added an online, "Virtual MS Center" to link you to professionals and other patients with the diverse skills and experiences required to help you and your provider effectively manage your MS over time. Starting today, we will begin asking you questions; after all, this is meant to be an interactive website; we cannot improve the site or our understanding of MS without your involvement. We need your active involvement if the site is going to grow and prosper. Spread the word and do it now! Please click on the link below to take the survey and help us create the best MS website for patients! Help us make the website the best it can be! -- Dr. Kinkel
This is a question I get several times a week and my answer has changed over time with the availability of newer therapies and more information on identifying individual risk factors for the development of Progressive Multifocal Leukoencephalopathy (PML), the complication of treatment with this highly effective drug that we are all trying to avoid. [If you do not know much about Tysabri or PML, I recommend you search our site for a refresher course and then return to this blog]. To better understand if Tysabri therapy is good for you, it is informative to take a short walk down memory lane. When Tysabri first returned to the market place in 2006 and MS specialists started treating patients under the TOUCH program, the risk of PML was estimated at 1/1000. Very quickly we learned about additional risks factors for PML; these new risk factors included,
This was followed by the development of a blood test to determine if your body was making antibodies against the virus that is associated with the development of PML, called the JC virus. Initially, results from the this blood test were reported as either positive or negative; those with a positive test (56% of people) seemed to have almost all the risk of developing PM, whereas those who were negative on this test (44%) had a negligible risk of developing PML. To make matters slightly more complicated, those who were negative on the JC virus antibody test could become positive later (about a 2% yearly conversion rate over the short term). The initial testing showed that about 40% of people with MS were negative on this test and 60% positive. For many neurologist and patients who were risk adverse, this eliminated Tysabri as a treatment option in at least 60% of patients who they felt were good candidates by other criteria. Around this time other highly effective therapies were becoming available for people with MS with their own set of risk factors, particularly Fingolimod (Gilenya) with its risk of cardiac complications, macular edema and reactivation of herpetic infections like shingles. We now have Tecfidera that appears relatively safe and effective, but associated with some unpleasant GI side effects in about 20% of people at the start of treatment. Thankfully, we have further refined the risk stratification for people wishing to consider Tysabri therapy and the FDA recently approved the use of Tysabri as a first line agent (people with no prior disease modifying therapy) in well selected relapsing MS patients. The main change in our risk stratification is based on a free test that measures the actual amount of antibodies your body makes against the JC virus, called the JC Virus antibody index. We no longer consider patients as simply positive or negative for JC antibodies. This new information on stratifying risk by JC virus index in addition to the prior known risk factors, which include duration of therapy and prior immunosuppressant use, forms the basis of assessing your risk of developing PML on Tysabri therapy. More importantly, the new risk stratification scheme reclassifies approximately 25% of the patients previously considered JC virus antibody positive as a relatively lower risk group who may now consider Tysabri therapy. Please see the attached figure to see the entire stratification scheme. Once you know your JC Virus index value (which you can get from your doctor) you can determine whether it is too risky for you to consider Tysabri by simply looking at the chart. First some highlights:
So how do I make these judgments? First, I think it is reasonable to consider an MS therapy as first line in almost all patients if a severe risk of that therapy occurs in less than 1 in 10,000 people. I would consider the therapy first line in selected patients with significant MS disease activity if the risk of PML were less than 1 in 2500 (see table. This would mean a JC virus index value of < 0.9). This is mostly because we have other therapies available that may work and have a lower risk profile. For higher risks of PML, I am inclined to consider therapy only as second or third line but will still use Tysabri in selected cases. So what is your risk profile? What are your thoughts on the risks associated with either Tysabri or any other MS disease modifying therapy? -- Dr. Kinkel PLEASE NOTE: The medical information on this site is provided as an information resource only, and is not to be used or relied on for any diagnostic or treatment purposes. The information and opinions provided do not create any patient-physician relationship, and should not be used as a substitute for professional diagnosis and treatment. Please consult your health care provider before making any healthcare decisions or for guidance about a specific medical condition. It seems fitting that on Valentine’s Day I should write about new hope for an MS treatment that may even benefit those with progressive disease! Better yet, this treatment may even target the cause of the disease instead of simply suppressing inflammatory responses within the central nervous system.
Researchers in Australia have published a case report documenting the rather dramatic response of a severe progressive MS patient to immunotherapy which was designed to boost a specific type of immune response against B Cells latently infected with Epstein Barr Virus, the cause of mononucleosis and a possible cause of MS. The patient experienced: · A dramatic reduction in inflammatory MRI lesions · Improvement in symptoms and neurological findings · A reduction in the production of immunoglobulins within the spinal fluid The reduction in immunoglobulin being produced within the nervous system and measured in spinal fluid was perhaps the most remarkable finding, as it suggests that this treatment eliminated intrathecal (meaning within the spinal fluid) B cells latently infected with Epstein Barr Virus. There is a wealth of direct and indirect evidence that Epstein Barr Virus plays an important role in causing MS. Pathological studies reveal nodules of inflammatory cells scattered across the surface of the brain, often in clusters resembling tiny lymph nodes. Many of these cells are a type of lymphocyte, called a B cell, that are infected with Epstein Barr virus. These inflammatory cells appear to directly damage the underlying cortex of the brain, which may trigger an inflammatory response that spreads throughout the nervous system over many years. It is these same B cells that mature to become the type of cells (called plasma cells) that produce the immunoglobulins in the spinal fluid (CSF) that we use to help diagnose MS. We call these immunoglobulins in the CSF oligoclonal bands. The therapy given to this patient was designed to boost the cytotoxic immune response against EBV infected B Cells. The immune system depends on cytoxic or CD8+ T immune cells to destroy cells infected with viruses, but this cytotoxic response is often lacking in MS patients. They used a novel approach to stimulate a sample of the patient’s blood with AdE1-LMPpoly, a recombinant adenovirus vector that boosts cytotoxic CD8+ T cell responses against Epstein Barr virus proteins expressed by infected B Cells, and then re-injected these boosted cells back into the patient. The patient tolerated the treatment well and improved. Clearly, these results require confirmation in well designed and controlled clinical trials, but for the first time we seem to have a path forward to finding an effective therapy for MS that is based on a reasonable hypothesis regarding the cause of the disease. I wouldn’t be surprised to find a therapy like this available within 5 years if confirmed by additional studies. Happy Valentine’s Day --Dr. Kinkel As you might have noticed, we are continuously making changes to this website to improve it. We have added our Virtual MS Center, the first we know of its kind. I will still be writing blogs from time to time for this 'physician blog,' but you will also want to visit (and bookmark) the "Q & A For Virtual MS Center" page as often as you can (click on the link below), as this will be where we post answers to questions coming in from people with MS.
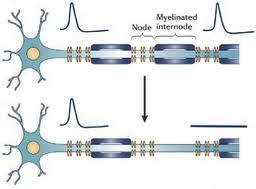
Abnormal Sensations in MS. Why do they occur and what do they mean? Abnormal sensations and pain are a common experience for people with MS. To understand this a little better, I need to begin with a short explanation of how the nervous system works. The images above are cross sectional depictions of two neurons and their associated axon. Neurons, as you can see, are strange looking cells with tentacles (axons and dendrites) that reach out and connect with other neurons in defined circuits. The connections made by these neurons are the means by which your nervous system receives information, interprets and manipulates information and acts on information. This information may come in the form of sights, sounds, tastes, smells, sensations or language. The information flow can also start from spontaneously generated thought and contemplation. The myelin that is damaged in MS is shown in blue (called the myelinated internode in the picture) wrapped around segments of the axon (shown in blue green) with gaps between the myelinated internode that are called the Nodes of Ranvier (labeled Node in the picture). As you may know it is common in medicine to name things after their founder and a French physician in the late 19th and early 20th century named Ranvier discovered this peculiar feature of our nervous systems. The top image is a normal neuron-axon unit and the lower image depicts a neuron-axon unit that has been stripped of myelin in an area but with no permanent damage to the axon. Now why is this a problem?
The difficult question is whether these new sodium channels that sprout all axons are harmful. There is some research that indicates that the effects of these sodium channels may lead to permanent damage to the neuron, but attempts so far to prevent this from occurring by administering drugs that block sodium channels have not been successful. At the end of the day, people really want to know what is causing their symptoms and how to manage them. Whether you have definite MS or not, there will always be some degree of uncertainty; uncertainty regarding your risk of MS, uncertainty regarding the risk of future relapses, uncertainty regarding the risk of developing disability and uncertainty regarding your response to therapy, whether it be a drug, a dietary charge or a lifestyle change. How you and your physician manage these uncertainties together over time defines the art of the doctor-patient relationship.
If this process doesn’t work for you with your current doctor, discuss it openly with him or her and, if necessary, find a new doctor. Try to figure out what it is you require from a doctor to help you manage your chronic condition. As in the rest of life there will always be compromises you have to make but try to decide what you find to be most essential. Practical issues such as insurance coverage and distance from the doctor’s office are certainly important when it comes to narrowing down the list of doctors to consider, but should not be the basis of your decision. To me a doctor must first take the time to listen and understand your narrative (doctors call this the “chief complaint”), ask probing questions, explain their interpretation of the information gathered to gain further feedback and information and then put together a plan of action that you are capable of understanding and that clearly addresses your initial complaints. This is much harder than it sounds since often the person describing the “complaint”, is not only unaware of the cause but also unaware of the influence of seemingly random or apparently unimportant aspects of their life on this complaint. To give an example, I am often asked by patients to help them with their daytime fatigue, probably the most common symptom of MS. Many patients simply assume they only need a medication for this complaint and have learned that other patients take various medications for their fatigue. In fact, the causes of fatigue are extremely difficult to unravel and require a skilled history and dedicated follow-up evaluations after testing, activity adjustments and possible medication intervention to arrive at a satisfactory solution. As with most problems in medicine this is an iterative process: First, the complaint is identified and understood as best as possible generating a hypothesis that involves further testing or an intervention; second, the patient is educated about the intervention and given the means to carry out the intervention and track the progress; third, the patient is re-evaluated to determine the initial outcome to the intervention and generate further hypotheses leading to further testing or interventions; etc. This process requires skill, time, empathy and interactive resources. Anyone with a chronic condition wants to find not only a good doctor but a doctor with the support staff and associated medical professionals dedicated to working together on finding individualized solutions to problems. In subsequent blogs we will be discussing these issues at length. I will always begin with the importance of education. Simply knowing the facts, or what is not known, is sometimes all that is needed. Where there are choices to be made I will try to outline them clearly, although it may become clear that I have a bias to express. Remember, an unbiased interpretation of data does not exist. What is important is whether the interpretation of the data is consistent with the known facts and your belief system. |
DISCLAIMER:
The medical information and opinions on this site are provided as an information resource only, and are not to be used or relied on for any diagnostic or treatment purposes. The information and opinions expressed do not create any patient-physician relationship, and should not be used as a substitute for professional diagnosis and treatment. Please consult your health care provider before making any healthcare decisions or for guidance about a specific medical condition. Archives
January 2020
Categories
All
|
- Home
- About Us
- Virtual MS Center
- News & Resources
- Seminar Registration
- Health & Wellness
- Blogs
- About MS
-
Symptoms
- Balance and Walking Issues
- Breathing/Respiratory
- Bowel Dysfunction
- Cognitive Dysfunction
- Crying/Laughing Uncontrollably (PBA)
- Depression and Anxiety
- Dizziness/Vertigo
- Dysphagia
- Fatigue
- Foot Drop
- Hearing or Smell or Taste Changes
- Heat Sensitivity
- Leg Weakness
- Loss of Hand Dexterity and Coordination
- Memory and Mutliple Sclerosis
- Migraines
- Numbness/Tingling/Altered Sensation
- Nystagmus and Oscillopsia
- Pain
- Sexual Dysfunction
- Sleep Issues
- Spasticity/Spasms/Cramps
- Speech/Swallowing
- Urination/Bowel Problems
- Vision
- MS Clinics
- MS Topics
- Register With Us
- Terms of Use/Privacy/HIPAA
- MS HealthCare Journey

 RSS Feed
RSS Feed
