Welcome to the Virtual MS Center!
Ask any question you want about Multiple Sclerosis and one of our experts will answer it as soon as possible.
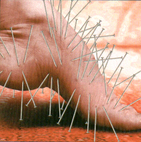 Question: I am 63 and have had MS for over 15 years. Recently I was told that my diagnosis is incorrect and that I really have small fiber neuropathy, not MS. I am so confused and need your advice. My symptoms began about 15 years ago with pins and needles sensations and burning in the feet. The symptoms would come and go and get worse in warm weather. Over time the symptoms became constant and then started all over my body. I also experience frequent odd jabbing and shock like sensations. Parts of my body are so painful to touch that having a sheet on me is unbearable. The original diagnosis of MS was made after an MRI scan of my head, but my spinal tap didn't show evidence of MS. I recently had another spinal tap by my new neurologist and it still didn't show any bands. I have been on Copaxone for years and wonder what I should do now? Answer: Your symptom description is typical of a small fiber neuropathy. While multiple sclerosis is known to cause odd sensations such as pins and needles, burning and electric shocks, these symptoms are hardly unique to MS and can be seen with any disorder that affects sensory pathways in the nervous system. Most individuals with MS will eventually develop more characteristic symptoms and findings on their exam, especially after 15 years. Since you did not mention any other non sensory symptoms or problems, I will assume that the neurologist who disagreed with the diagnosis of MS did not find any of these abnormalities. It is also not uncommon to misinterpret non specific “white spots” on MRI scans as evidence of MS. The community of MS specialists has developed partially effective descriptors of MRI abnormalities that are more typical of MS, but many neurologists and radiologists remain unaware of these guidelines. The normal spinal fluid results, especially if repeated over time, is important. Very few individuals have CSF negative Multiple Sclerosis after so many years of symptoms. Small Fiber Neuropathy is a condition selectively affecting the small unmyelinated, peripheral sensory nerves that relay information concerning pain and temperature to your brain. This type of neuropathy has many causes including diabetes and medications (cancer drugs) but a cause is never found in up to half of individuals affected with this disorder. At times people with small fiber neuropathy will have symptoms of autonomic dysfunction including dry eyes and mouth, lightheadedness on standing or spells of syncope, irregular heart beats, problems with sweating, urinary incontinence and erectile dysfunction. The diagnosis is made by a careful history and exam usually confirmed by a punch biopsy of the skin to examine the small sensory density of nerve endings under a microscope. Needless to say, the medications used to treat MS are not effective for this condition and should be discontinued. Even if an underlying cause is found, treatment consists primarily of various medications to block or modify the painful sensations. The medications commonly to accomplish this goal include the anticonvulsant class of drugs (gabapentin, pregabalin, carbamezipine, oxcarbezipine, lamotrigine and phenytoin to name a few), topical agents (lidocaine patches and capsaicin) and the tricyclic antidepressant class of medications and more modern alternatives (amitriptyline, venlafaxine and duloxetine). Revere (Rip) Kinkle Director of the UCSD Multiple Sclerosis Center PLEASE NOTE: The information/opinions on this site should be used as an information resource only. This information does not create any patient-HCP relationship, and should not be used as a substitute for professional diagnosis and treatment. Please consult your health care provider before making any healthcare decisions or for guidance about a specific medical condition.
Szollar
8/5/2016 06:38:05 pm
This information was very helpful and easily understood..thank you!
Kay jones
1/11/2018 09:46:39 am
I was diagnosed with SFN several yrs ago after 3 different spinal taps over a span of 6 yrs. Each time the Doctors kept saying you don’t have MS. The leasions in my brain are growing like MS but not MS. I was finally sent to Houston to a neurologist for a skin and muscle biopsy. That is where my final diagnosis came. Never to work again because of balance problems becoming a liability.. I just learn to live day to day. 4/26/2018 11:47:44 am
After seeing a neuro-optomologist, I was given a diagnosis of trigeminal neuralgia. I was told it was just facial nerve pain. Over the last six years, I've had 4 different doctor's say it appears that I am suffering from an underlying issue. However, I am suffering from severe nerve pain and chronic inflammation all over. Neurologists have refused to run any tests to rule out any neurological disorders inspite of my multitude of positive tests for multiple conditions. I have recently read up on MS when reading about the nerve disorder. My neuropathy was only on my feet and over the last few years has grown to encompass my entire body. In the last few months, I've acquired more new joint pain in my hands and arms and now my knees ache as well. I have constantly gone through major episodes or relapses of chronic inflammation all over to the point I need an injection of a strong muscle relaxer (non-steroid) to calm the inflammation as it's uncontrollable per my daily regime. My immune system is shot. I survive off a daily sinus regime in order to breathe as I my passages will flame and make breathing difficult. I need to know what tests to demand and fully disclose as to a proper diagnosis to determine of I have MS. I have more conditions that have steadily grown into more problems as well.
Janine Langan
5/7/2018 06:22:03 am
My symtoms are similar i have been passed from pillor to post its awful. Had skin biopsy to confirm snf. Now specalist said he will find out why. He is really good. Comments are closed.
|
PLEASE NOTE: This information/opinions on this site should be used as an information source only. This information does not create any patient-HCP relationship, and should not be used as a substitute for professional diagnosis and treatment. Please consult your health care provider before making any healthcare decisions or for guidance about a specific medical condition.
Archives
March 2024
Categories
All
|